Dermatitis is inflammation of the skin, typically characterized by itchiness, redness and a rash. In cases of short duration, there may be small blisters, while in long-term cases the skin may become thickened. The area of skin involved can vary from small to covering the entire body. Dermatitis is often called eczema, and the difference between those terms is not standardized.

Psoriasis is a long-lasting, noncontagious autoimmune disease characterized by patches of abnormal skin. These areas are red, pink, or purple, dry, itchy, and scaly. Psoriasis varies in severity from small localized patches to complete body coverage. Injury to the skin can trigger psoriatic skin changes at that spot, which is known as the Koebner phenomenon.

Tinea versicolor is a condition characterized by a skin eruption on the trunk and proximal extremities. The majority of tinea versicolor is caused by the fungus Malassezia globosa, although Malassezia furfur is responsible for a small number of cases. These yeasts are normally found on the human skin and become troublesome only under certain circumstances, such as a warm and humid environment, although the exact conditions that cause initiation of the disease process are poorly understood.

Itch is a sensation that causes a strong desire or reflex to scratch. Itches have resisted many attempts to be classified as any one type of sensory experience. Itches have many similarities to pain, and while both are unpleasant sensory experiences, their behavioral response patterns are different. Pain creates a withdrawal reflex, whereas itches leads to a scratch reflex.

Seborrhoeic dermatitis is a long-term skin disorder. Symptoms include flaky, scaly, greasy, and occasionally itchy and inflamed skin. Areas of the skin rich in oil-producing glands are often affected including the scalp, face, and chest. It can result in social or self-esteem problems. In babies, when the scalp is primarily involved, it is called cradle cap. Seborrhoeic dermatitis of the scalp may be described in lay terms as dandruff due to the dry, flaky character of the skin. However, as dandruff may refer to any dryness or scaling of the scalp, not all dandruff is seborrhoeic dermatitis. Seborrhoeic dermatitis is sometimes inaccurately referred to as seborrhoea.

Ichthyosis vulgaris is a skin disorder causing dry, scaly skin. It is the most common form, and one of the mildest forms, of ichthyosis, affecting around 1 in 250 people. For this reason it is known as common ichthyosis. It is usually an autosomal dominant inherited disease, although a rare non-heritable version called acquired ichthyosis exists.

Pimecrolimus is an immunomodulating agent of the calcineurin inhibitor class used in the treatment of atopic dermatitis (eczema). It is available as a topical cream, once marketed by Novartis under the trade name Elidel.

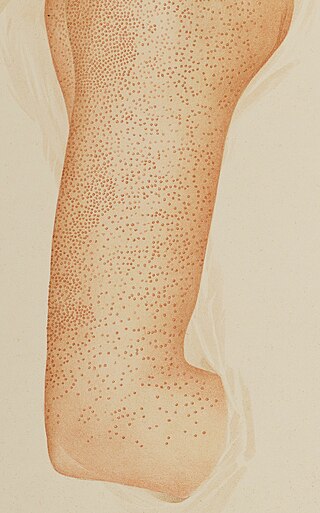
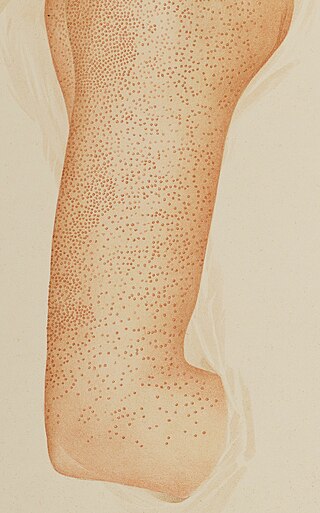
Keratosis pilaris is a common, autosomal-dominant, genetic condition of the skin's hair follicles characterized by the appearance of possibly itchy, small, gooseflesh-like bumps, with varying degrees of reddening or inflammation. It most often appears on the outer sides of the upper arms, thighs, face, back, and buttocks; KP can also occur on the hands, and tops of legs, sides, or any body part except glabrous (hairless) skin. Often the lesions can appear on the face, which may be mistaken for acne or folliculitis.

Mycosis fungoides, also known as Alibert-Bazin syndrome or granuloma fungoides, is the most common form of cutaneous T-cell lymphoma. It generally affects the skin, but may progress internally over time. Symptoms include rash, tumors, skin lesions, and itchy skin.

Cutaneous T-cell lymphoma (CTCL) is a class of non-Hodgkin lymphoma, which is a type of cancer of the immune system. Unlike most non-Hodgkin lymphomas, CTCL is caused by a mutation of T cells. The cancerous T cells in the body initially migrate to the skin, causing various lesions to appear. These lesions change shape as the disease progresses, typically beginning as what appears to be a rash which can be very itchy and eventually forming plaques and tumors before spreading to other parts of the body.

Desonide (INN) is a low-potency topical corticosteroid anti-inflammatory that has been available since the 1970s. It is primarily used to treat atopic dermatitis (eczema), seborrheic dermatitis, contact dermatitis and psoriasis in both adults and children. It has a fairly good safety profile and is available as a cream, ointment, lotion, and as a foam under the tradename Verdeso Foam. Other trade names for creams, lotions, and ointments include Tridesilon, DesOwen, Desonate. It is a group VI corticosteroid under US classification, the second least potent group.
Pityriasis rubra pilaris refers to a group of chronic disorders characterized by reddish orange, scaling plaques and keratotic follicular papules. Symptoms may include reddish-orange patches on the skin, severe flaking, uncomfortable itching, thickening of the skin on the feet and hands, and thickened bumps around hair follicles. For some, early symptoms may also include generalized swelling of the legs, feet and other parts of the body. PRP has a varied clinical progression and a varied rate of improvement. There is currently no known cause or cure for PRP.
Selenium disulfide, also known as selenium sulfide, is a chemical compound and medication used to treat seborrheic dermatitis, dandruff, and pityriasis versicolor. It is applied to the affected area as a lotion or shampoo. Symptoms frequently return if treatment is stopped.

Prurigo nodularis (PN), also known as nodular prurigo, is a skin disease characterised by pruritic (itchy) nodules which usually appear on the arms or legs. Patients often present with multiple excoriated lesions caused by scratching. PN is also known as Hyde prurigo nodularis, Picker's nodules, atypical nodular form of neurodermatitis circumscripta, lichen corneus obtusus.

The Koebner phenomenon or Köbner phenomenon, also called the Koebner response or the isomorphic response, attributed to Heinrich Köbner, is the appearance of skin lesions on lines of trauma. The Koebner phenomenon may result from either a linear exposure or irritation. Conditions demonstrating linear lesions after a linear exposure to a causative agent include: molluscum contagiosum, warts and toxicodendron dermatitis. Warts and molluscum contagiosum lesions can be spread in linear patterns by self-scratching ("auto-inoculation"). Toxicodendron dermatitis lesions are often linear from brushing up against the plant. Causes of the Koebner phenomenon that are secondary to scratching rather than an infective or chemical cause include vitiligo, psoriasis, lichen planus, lichen nitidus, pityriasis rubra pilaris, and keratosis follicularis.
Trichorrhexis invaginata is a distinctive hair shaft abnormality that may occur sporadically, either in normal hair or with other hair shaft abnormalities, or regularly as a marker for Netherton syndrome. The primary defect appears to be abnormal keratinization of the hair shaft in the keratogenous zone, allowing for intussusception of the fully keratinized and hard distal shaft into the incompletely keratinized and soft proximal portion of the shaft.

Pityriasis amiantacea is an eczematous condition of the scalp in which thick tenaciously adherent scale infiltrates and surrounds the base of a group of scalp hairs. It does not result in scarring or alopecia.

Onychauxis presents with thickened nails without deformity, and this simple thickening may be the result of trauma, acromegaly, Darier's disease, psoriasis, or pityriasis rubra pilaris, or, in some cases, hereditary.
Senile pruritus is one of the most common conditions in the elderly or people over 65 years of age with an emerging itch that may be accompanied with changes in temperature and textural characteristics. In the elderly, xerosis, is the most common cause for an itch due to the degradation of the skin barrier over time. However, the cause of senile pruritus is not clearly known. Diagnosis is based on an elimination criteria during a full body examination that can be done by either a dermatologist or non-dermatologist physician.