Carpal tunnel syndrome (CTS) is the collection of symptoms and signs associated with nerve compression of the median nerve at the carpal tunnel. Most CTS is related to idiopathic compression of the median nerve as it travels through the wrist at the carpal tunnel. Idiopathic means that there is no other disease process contributing to pressure on the nerve. As with most structural issues, it occurs in both hands, and the strongest risk factor is genetics.

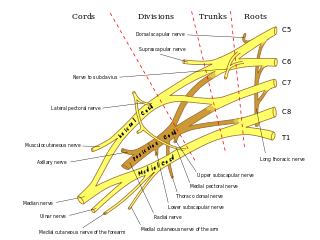
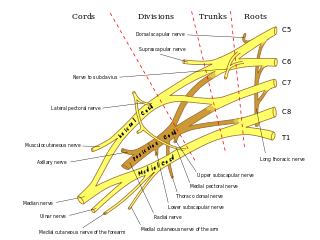
The median nerve is a nerve in humans and other animals in the upper limb. It is one of the five main nerves originating from the brachial plexus.
In human anatomy, the ulnar nerve is a nerve that runs near the ulna bone. The ulnar collateral ligament of elbow joint is in relation with the ulnar nerve. The nerve is the largest in the human body unprotected by muscle or bone, so injury is common. This nerve is directly connected to the little finger, and the adjacent half of the ring finger, innervating the palmar aspect of these fingers, including both front and back of the tips, perhaps as far back as the fingernail beds.

A nerve conduction study (NCS) is a medical diagnostic test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body. These tests may be performed by medical specialists such as clinical neurophysiologists, physical therapists, physiatrists, and neurologists who subspecialize in electrodiagnostic medicine. In the United States, neurologists and physiatrists receive training in electrodiagnostic medicine as part of residency training and in some cases acquire additional expertise during a fellowship in clinical neurophysiology, electrodiagnostic medicine, or neuromuscular medicine. Outside the US, clinical neurophysiologists learn needle EMG and NCS testing.
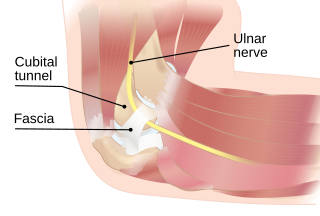
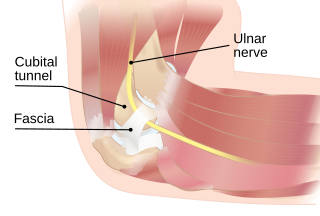
The cubital tunnel is a space of the dorsal medial elbow which allows passage of the ulnar nerve around the elbow. It is bordered medially by the medial epicondyle of the humerus, laterally by the olecranon process of the ulna and the tendinous arch joining the humeral and ulnar heads of the flexor carpi ulnaris. The roof of the cubital tunnel is elastic and formed by a myofascial trilaminar retinaculum. In 14% of individuals, the roof of this tunnel is covered by epitrochleoanconeus muscle, a variant muscle.

Tarsal tunnel syndrome (TTS) is a nerve entrapment syndrome causing a painful foot condition in which the tibial nerve is compressed as it travels through the tarsal tunnel. This tunnel is found along the inner leg behind the medial malleolus. The posterior tibial artery, tibial nerve, and tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles travel in a bundle through the tarsal tunnel. Inside the tunnel, the nerve splits into three segments. One nerve (calcaneal) continues to the heel, the other two continue on to the bottom of the foot. The tarsal tunnel is delineated by bone on the inside and the flexor retinaculum on the outside.

In neuroscience, nerve conduction velocity (CV) is the speed at which an electrochemical impulse propagates down a neural pathway. Conduction velocities are affected by a wide array of factors, which include age, sex, and various medical conditions. Studies allow for better diagnoses of various neuropathies, especially demyelinating diseases as these conditions result in reduced or non-existent conduction velocities. CV is an important aspect of nerve conduction studies.

The flexor retinaculum is a fibrous band on the palmar side of the hand near the wrist. It arches over the carpal bones of the hands, covering them and forming the carpal tunnel.

The ulnar canal or ulnar tunnel (also known as Guyon's canal or tunnel) is a semi-rigid longitudinal canal in the wrist that allows passage of the ulnar artery and ulnar nerve into the hand. The roof of the canal is made up of the superficial palmar carpal ligament, while the deeper flexor retinaculum and hypothenar muscles comprise the floor. The space is medially bounded by the pisiform and pisohamate ligament more proximally, and laterally bounded by the hook of the hamate more distally. It is approximately 4 cm long, beginning proximally at the transverse carpal ligament and ending at the aponeurotic arch of the hypothenar muscles.

In the human body, the carpal tunnel or carpal canal is a flattened body cavity on the flexor (palmar/volar) side of the wrist, bounded by the carpal bones and flexor retinaculum. It forms the passageway that transmits the median nerve and the tendons of the extrinsic flexor muscles of the hand from the forearm to the hand. There are described cases of the anatomical variant median artery occurrence.

Idiopathic Ulnar neuropathy at the elbow is a condition where pressure on the ulnar nerve as it passes through the cubital tunnel causes nerve dysfunction (neuropathy). The symptoms of neuropathy are paresthesia (tingling) and numbness primarily affecting the little finger and ring finger of the hand. Ulnar neuropathy can progress to weakness and atrophy of the muscles in the hand. Symptoms can be alleviated by attempts to keep the elbow from flexing while sleeping, such as sticking one's arm in the pillow case, so the pillow restricts flexion.

Ulnar neuropathy is a disorder involving the ulnar nerve. Ulnar neuropathy may be caused by entrapment of the ulnar nerve with resultant numbness and tingling. It may also cause weakness or paralysis of the muscles supplied by the nerve.

Nerve compression syndrome, or compression neuropathy, or nerve entrapment syndrome, is a medical condition caused by chronic, direct pressure on a peripheral nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression. Its symptoms include pain, tingling, numbness and muscle weakness. The symptoms affect just one particular part of the body, depending on which nerve is affected. The diagnosis is largely clinical and can be confirmed with diagnostic nerve blocks. Occasionally imaging and electrophysiology studies aid in the diagnosis. Timely diagnosis is important as untreated chronic nerve compression may cause permanent damage. A surgical nerve decompression can relieve pressure on the nerve but cannot always reverse the physiological changes that occurred before treatment. Nerve injury by a single episode of physical trauma is in one sense an acute compression neuropathy but is not usually included under this heading, as chronic compression takes a unique pathophysiological course.

Wrist pain or open wrist is a type of syndrome that prevents the patient using their hand due to a painful wrist. The pain may be sharp, sometimes steadily increasing after trying to apply force. Typically pain is caused after exerting too strong a demand on the wrist, as is the case with weight lifters, athletes in general, or with any weight-bearing activity to the wrist.
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi.

Injuries to the arm, forearm or wrist area can lead to various nerve disorders. One such disorder is median nerve palsy. The median nerve controls the majority of the muscles in the forearm. It controls abduction of the thumb, flexion of hand at wrist, flexion of digital phalanx of the fingers, is the sensory nerve for the first three fingers, etc. Because of this major role of the median nerve, it is also called the eye of the hand. If the median nerve is damaged, the ability to abduct and oppose the thumb may be lost due to paralysis of the thenar muscles. Various other symptoms can occur which may be repaired through surgery and tendon transfers. Tendon transfers have been very successful in restoring motor function and improving functional outcomes in patients with median nerve palsy.

Carpal tunnel surgery, also called carpal tunnel release (CTR) and carpal tunnel decompression surgery, is a nerve decompression in which the transverse carpal ligament is divided. It is a surgical treatment for carpal tunnel syndrome (CTS) and recommended when there is constant (not just intermittent) numbness, muscle weakness, or atrophy, and when night-splinting no longer controls intermittent symptoms of pain in the carpal tunnel. In general, milder cases can be controlled for months to years, but severe cases are unrelenting symptomatically and are likely to result in surgical treatment. Approximately 500,000 surgical procedures are performed each year, and the economic impact of this condition is estimated to exceed $2 billion annually.
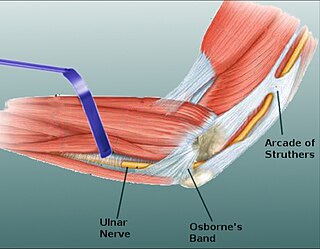
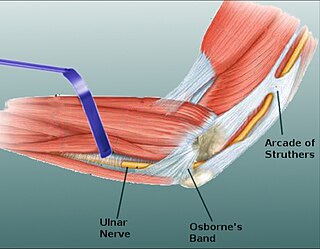
Osborne's ligament, also Osborne's band, Osborne's fascia, Osborne's arcade, arcuate ligament of Osborne, or the cubital tunnel retinaculum, refers to either the connective tissue which spans the humeral and ulnar heads of the flexor carpi ulnaris (FCU) or another distinct tissue located between the olecranon process of the ulna and the medial epicondyle of the humerus. It is named after Geoffrey Vaughan Osborne, a British orthopedic surgeon, who described the eponymous tissue in 1957.
Nerve glide, also known as nerve flossing or nerve stretching, is an exercise that stretches nerves. It facilitates the smooth and regular movement of peripheral nerves in the body. It allows the nerve to glide freely along with the movement of the joint and relax the nerve from compression. Nerve gliding cannot proceed with injuries or inflammations as the nerve is trapped by the tissue surrounding the nerve near the joint. Thus, nerve gliding exercise is widely used in rehabilitation programs and during the post-surgical period.