Keratoconus (KC) is a disorder of the eye that results in progressive thinning of the cornea. This may result in blurry vision, double vision, nearsightedness, irregular astigmatism, and light sensitivity leading to poor quality-of-life. Usually both eyes are affected. In more severe cases a scarring or a circle may be seen within the cornea.

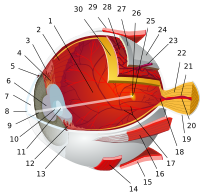
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Along with the anterior chamber and lens, the cornea refracts light, accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.
A microkeratome is a precision surgical instrument with an oscillating blade designed for creating the corneal flap in LASIK or ALK surgery. The normal human cornea varies from around 500 to 600 micrometres in thickness; and in the LASIK procedure, the microkeratome creates an 83 to 200 micrometre thick flap. This piece of equipment is used all around the world to cut the cornea flap. The microkeratome is also used in Descemet's stripping automated endothelial keratoplasty (DSAEK), where it is used to slice a thin layer from the back of the donor cornea, which is then transplanted into the posterior cornea of the recipient. It was invented by Jose Barraquer and Cesar Carlos Carriazo in the 1950s in Colombia.

The Bowman's layer is a smooth, acellular, nonregenerating layer, located between the superficial epithelium and the stroma in the cornea of the eye. It is composed of strong, randomly oriented collagen fibrils in which the smooth anterior surface faces the epithelial basement membrane and the posterior surface merges with the collagen lamellae of the corneal stroma proper.

The corneal endothelium is a single layer of endothelial cells on the inner surface of the cornea. It faces the chamber formed between the cornea and the iris.
The basal lamina is a layer of extracellular matrix secreted by the epithelial cells, on which the epithelium sits. It is often incorrectly referred to as the basement membrane, though it does constitute a portion of the basement membrane. The basal lamina is visible only with the electron microscope, where it appears as an electron-dense layer that is 20–100 nm thick.

Corneal transplantation, also known as corneal grafting, is a surgical procedure where a damaged or diseased cornea is replaced by donated corneal tissue. When the entire cornea is replaced it is known as penetrating keratoplasty and when only part of the cornea is replaced it is known as lamellar keratoplasty. Keratoplasty simply means surgery to the cornea. The graft is taken from a recently deceased individual with no known diseases or other factors that may affect the chance of survival of the donated tissue or the health of the recipient.

Fuchs dystrophy, also referred to as Fuchs endothelial corneal dystrophy (FECD) and Fuchs endothelial dystrophy (FED), is a slowly progressing corneal dystrophy that usually affects both eyes and is slightly more common in women than in men. Although early signs of Fuchs dystrophy are sometimes seen in people in their 30s and 40s, the disease rarely affects vision until people reach their 50s and 60s.

A corneal ulcer, or ulcerative keratitis, is an inflammatory condition of the cornea involving loss of its outer layer. It is very common in dogs and is sometimes seen in cats. In veterinary medicine, the term corneal ulcer is a generic name for any condition involving the loss of the outer layer of the cornea, and as such is used to describe conditions with both inflammatory and traumatic causes.

Corneal dystrophy is a group of rare hereditary disorders characterised by bilateral abnormal deposition of substances in the transparent front part of the eye called the cornea.

The stroma of the cornea is a fibrous, tough, unyielding, perfectly transparent and the thickest layer of the cornea of the eye. It is between Bowman's layer anteriorly, and Descemet's membrane posteriorly.

The corneal epithelium is made up of epithelial tissue and covers the front of the cornea. It acts as a barrier to protect the cornea, resisting the free flow of fluids from the tears, and prevents bacteria from entering the epithelium and corneal stroma.

Bullous keratopathy, also known as pseudophakic bullous keratopathy (PBK), is a pathological condition in which small vesicles, or bullae, are formed in the cornea due to endothelial dysfunction.

Congenital hereditary corneal dystrophy (CHED) is a form of corneal endothelial dystrophy that presents at birth.
Dua's layer, according to a 2013 paper by Harminder Singh Dua's group at the University of Nottingham, is a layer of the cornea that had not been detected previously. It is hypothetically 15 micrometres thick, the fourth caudal layer, and located between the corneal stroma and Descemet's membrane. Despite its thinness, the layer is very strong and impervious to air. It is strong enough to withstand up to 2 bars of pressure. While some scientists welcomed the announcement, other scientists cautioned that time was needed for other researchers to confirm the discovery and its significance. Others have met the claim "with incredulity".

Corneal hydrops is an uncommon complication seen in people with advanced keratoconus or other corneal ectatic disorders, and is characterized by stromal edema due to leakage of aqueous humor through a tear in Descemet's membrane. Although a hydrops usually causes increased scarring of the cornea, occasionally it will benefit a patient by creating a flatter cone, aiding the fitting of contact lenses. Corneal transplantation is not usually indicated during corneal hydrops.
Pre Descemet's endothelial keratoplasty (PDEK) is a kind of endothelial keratoplasty, where the pre descemet's layer (PDL) along with descemet's membrane (DM) and endothelium is transplanted. Conventionally in a corneal transplantation, doctors use a whole cornea or parts of the five layers of the cornea to perform correction surgeries. In May 2013, Dr Harminder Dua discovered a sixth layer between the stroma and the descemet membrane which was named after him as the Dua's layer. In the PDEK technique, doctors take the innermost two layers of the cornea, along with the Dua's layer and graft it in the patient's eye.

In ophthalmology, glued intraocular lens or glued IOL is a surgical technique for implantation, with the use of biological glue, of a posterior chamber IOL in eyes with deficient or absent posterior capsules. A quick-acting surgical fibrin sealant derived from human blood plasma, with both hemostatic and adhesive properties, is used.
Descemet membrane endothelial keratoplasty (DMEK) is a method of corneal transplantation. The DMEK technique involves the removal of a very thin sheet of tissue from the posterior side of a person's cornea, replacing it with the two innermost layers of corneal tissue from a donor's eyeball. The two corneal layers which are exchanged are the Descemet's membrane and the corneal endothelium. The person's corneal tissue is gently excised and replaced with the donor tissue via small 'clear corneal incisions' (small corneal incisions just anterior to the corneal limbus. The donor tissue is tamponaded against the person's exposed posterior corneal stroma by injecting a small air bubble into the anterior chamber. To ensure the air tamponade is effective, it is necessary for people to strictly posture so that they are looking up at the ceiling during the recovery period and until the air bubble has fully resorbed.

The human cornea is a transparent membrane which allows light to pass through it. The word corneal opacification literally means loss of normal transparency of cornea. The term corneal opacity is used particularly for the loss of transparency of cornea due to scarring. Transparency of the cornea is dependent on the uniform diameter and the regular spacing and arrangement of the collagen fibrils within the stroma. Alterations in the spacing of collagen fibrils in a variety of conditions including corneal edema, scars, and macular corneal dystrophy is clinically manifested as corneal opacity. The term corneal blindness is commonly used to describe blindness due to corneal opacity.
Histology A text and atlas. Michael H.Ross and Wojciech Pawlina 5th Edition 2006