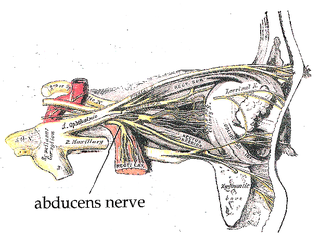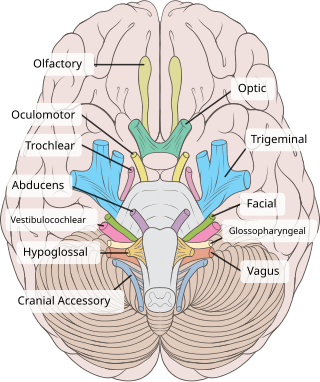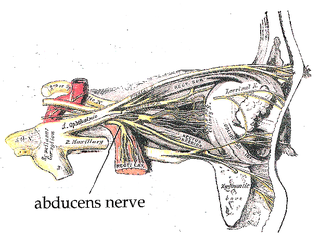
The abducens nerve or abducent nerve, also known as the sixth cranial nerve, cranial nerve VI, or simply CN VI, is a cranial nerve in humans and various other animals that controls the movement of the lateral rectus muscle, one of the extraocular muscles responsible for outward gaze. It is a somatic efferent nerve.
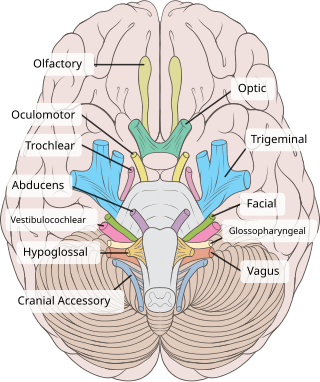
The oculomotor nerve, also known as the third cranial nerve, cranial nerve III, or simply CN III, is a cranial nerve that enters the orbit through the superior orbital fissure and innervates extraocular muscles that enable most movements of the eye and that raise the eyelid. The nerve also contains fibers that innervate the intrinsic eye muscles that enable pupillary constriction and accommodation. The oculomotor nerve is derived from the basal plate of the embryonic midbrain. Cranial nerves IV and VI also participate in control of eye movement.

In anatomy, the orbit is the cavity or socket/hole of the skull in which the eye and its appendages are situated. "Orbit" can refer to the bony socket, or it can also be used to imply the contents. In the adult human, the volume of the orbit is 30 millilitres, of which the eye occupies 6.5 ml. The orbital contents comprise the eye, the orbital and retrobulbar fascia, extraocular muscles, cranial nerves II, III, IV, V, and VI, blood vessels, fat, the lacrimal gland with its sac and duct, the eyelids, medial and lateral palpebral ligaments, cheek ligaments, the suspensory ligament, septum, ciliary ganglion and short ciliary nerves.
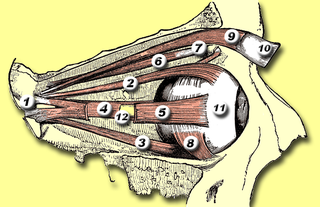
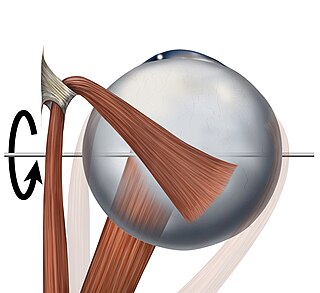
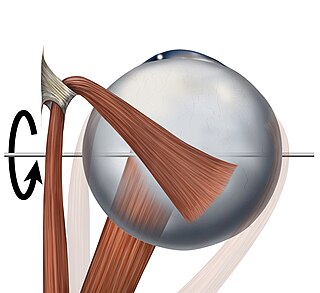
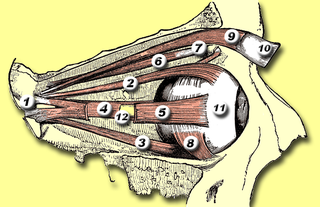
The superior oblique muscle or obliquus oculi superior is a fusiform muscle originating in the upper, medial side of the orbit which abducts, depresses and internally rotates the eye. It is the only extraocular muscle innervated by the trochlear nerve.
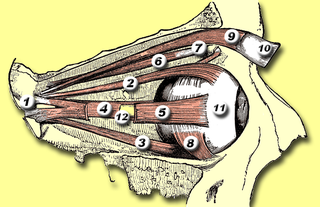
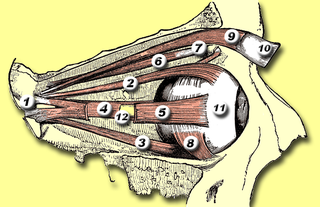
The levator palpebrae superioris is the muscle in the orbit that elevates the upper eyelid.

The superior rectus muscle is a muscle in the orbit. It is one of the extraocular muscles. It is innervated by the superior division of the oculomotor nerve (III). In the primary position, its primary function is elevation, although it also contributes to intorsion and adduction. It is associated with a number of medical conditions, and may be weak, paralysed, overreactive, or even congenitally absent in some people.
The inferior rectus muscle is a muscle in the orbit near the eye. It is one of the four recti muscles in the group of extraocular muscles. It originates from the common tendinous ring, and inserts into the anteroinferior surface of the eye. It depresses the eye (downwards).

The lateral rectus muscle is a muscle on the lateral side of the eye in the orbit. It is one of six extraocular muscles that control the movements of the eye. The lateral rectus muscle is responsible for lateral movement of the eyeball, specifically abduction. Abduction describes the movement of the eye away from the midline, allowing the eyeball to move horizontally in the lateral direction, bringing the pupil away from the midline of the body.
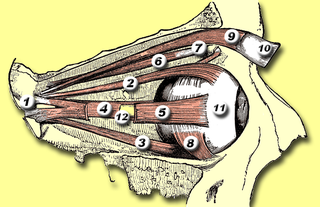
The inferior oblique muscle or obliquus oculi inferior is a thin, narrow muscle placed near the anterior margin of the floor of the orbit. The inferior oblique is one of the extraocular muscles, and is attached to the maxillary bone (origin) and the posterior, inferior, lateral surface of the eye (insertion). The inferior oblique is innervated by the inferior branch of the oculomotor nerve.

The extraocular muscles, or extrinsic ocular muscles, are the seven extrinsic muscles of the eye in humans and other animals. Six of the extraocular muscles, the four recti muscles, and the superior and inferior oblique muscles, control movement of the eye. The other muscle, the levator palpebrae superioris, controls eyelid elevation. The actions of the six muscles responsible for eye movement depend on the position of the eye at the time of muscle contraction.
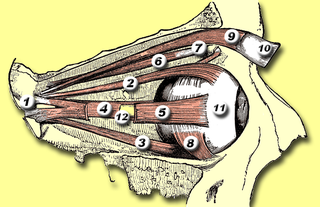
The common tendinous ring, also known as the annulus of Zinn or annular tendon, is a ring of fibrous tissue surrounding the optic nerve at its entrance at the apex of the orbit. It is the common origin of the four recti muscles of the group of extraocular muscles.
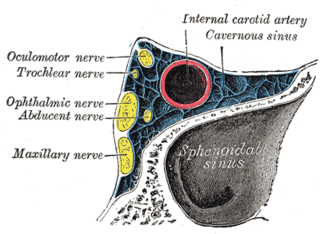
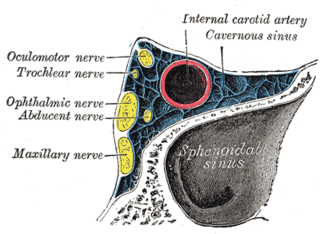
The ophthalmic nerve (CN V1) is a sensory nerve of the head. It is one of three divisions of the trigeminal nerve (CN V), a cranial nerve. It has three major branches which provide sensory innervation to the eye, and the skin of the upper face and anterior scalp, as well as other structures of the head.

The nasociliary nerve is a branch of the ophthalmic nerve (CN V1) (which is in turn a branch of the trigeminal nerve (CN V)). It is intermediate in size between the other two branches of the ophthalmic nerve, the frontal nerve and lacrimal nerve.

Sixth nerve palsy, or abducens nerve palsy, is a disorder associated with dysfunction of cranial nerve VI, which is responsible for causing contraction of the lateral rectus muscle to abduct the eye. The inability of an eye to turn outward, results in a convergent strabismus or esotropia of which the primary symptom is diplopia in which the two images appear side-by-side. Thus, the diplopia is horizontal and worse in the distance. Diplopia is also increased on looking to the affected side and is partly caused by overaction of the medial rectus on the unaffected side as it tries to provide the extra innervation to the affected lateral rectus. These two muscles are synergists or "yoke muscles" as both attempt to move the eye over to the left or right. The condition is commonly unilateral but can also occur bilaterally.

The supratrochlear nerve is a branch of the frontal nerve, itself a branch of the ophthalmic nerve (CN V1) from the trigeminal nerve (CN V). It provides sensory innervation to the skin of the forehead and the upper eyelid.
The trochlea of superior oblique is a pulley-like structure in the eye. The tendon of the superior oblique muscle passes through it. Situated on the superior nasal aspect of the frontal bone, it is the only cartilage found in the normal orbit. The word trochlea comes from the Greek word for pulley.

Strabismus surgery is surgery on the extraocular muscles to correct strabismus, the misalignment of the eyes. Strabismus surgery is a one-day procedure that is usually performed under general anesthesia most commonly by either a neuro- or pediatric ophthalmologist. The patient spends only a few hours in the hospital with minimal preoperative preparation. After surgery, the patient should expect soreness and redness but is generally free to return home.

An orbital blowout fracture is a traumatic deformity of the orbital floor or medial wall that typically results from the impact of a blunt object larger than the orbital aperture, or eye socket. Most commonly this results in a herniation of orbital contents through the orbital fractures. The proximity of maxillary and ethmoidal sinus increases the susceptibility of the floor and medial wall for the orbital blowout fracture in these anatomical sites. Most commonly, the inferior orbital wall, or the floor, is likely to collapse, because the bones of the roof and lateral walls are robust. Although the bone forming the medial wall is the thinnest, it is buttressed by the bone separating the ethmoidal air cells. The comparatively thin bone of the floor of the orbit and roof of the maxillary sinus has no support and so the inferior wall collapses mostly. Therefore, medial wall blowout fractures are the second-most common, and superior wall, or roof and lateral wall, blowout fractures are uncommon and rare, respectively. They are characterized by double vision, sunken ocular globes, and loss of sensation of the cheek and upper gums from infraorbital nerve injury.
Botulinum toxin therapy of strabismus is a medical technique used sometimes in the management of strabismus, in which botulinum toxin is injected into selected extraocular muscles in order to reduce the misalignment of the eyes. The injection of the toxin to treat strabismus, reported upon in 1981, is considered to be the first ever use of botulinum toxin for therapeutic purposes. Today, the injection of botulinum toxin into the muscles that surround the eyes is one of the available options in the management of strabismus. Other options for strabismus management are vision therapy and occlusion therapy, corrective glasses and prism glasses, and strabismus surgery.
The management of strabismus may include the use of drugs or surgery to correct the strabismus. Agents used include paralytic agents such as botox used on extraocular muscles, topical autonomic nervous system agents to alter the refractive index in the eyes, and agents that act in the central nervous system to correct amblyopia.