The thyroid, or thyroid gland, is an endocrine gland in vertebrates. In humans, it is in the neck and consists of two connected lobes. The lower two thirds of the lobes are connected by a thin band of tissue called the isthmus (pl.: isthmi). The thyroid gland is a butterfly-shaped gland located in the neck below the Adam's apple. Microscopically, the functional unit of the thyroid gland is the spherical thyroid follicle, lined with follicular cells (thyrocytes), and occasional parafollicular cells that surround a lumen containing colloid. The thyroid gland secretes three hormones: the two thyroid hormones – triiodothyronine (T3) and thyroxine (T4) – and a peptide hormone, calcitonin. The thyroid hormones influence the metabolic rate and protein synthesis and growth and development in children. Calcitonin plays a role in calcium homeostasis. Secretion of the two thyroid hormones is regulated by thyroid-stimulating hormone (TSH), which is secreted from the anterior pituitary gland. TSH is regulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus.
Hypothyroidism is a disorder of the endocrine system in which the thyroid gland does not produce enough thyroid hormones. It can cause a number of symptoms, such as poor ability to tolerate cold, a feeling of tiredness, constipation, slow heart rate, depression, and weight gain. Occasionally there may be swelling of the front part of the neck due to goitre. Untreated cases of hypothyroidism during pregnancy can lead to delays in growth and intellectual development in the baby or congenital iodine deficiency syndrome.

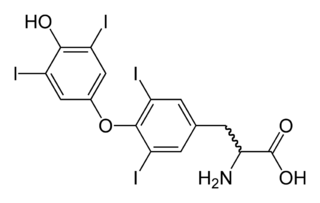
Iodothyronine deiodinases (EC 1.21.99.4 and EC 1.21.99.3) are a subfamily of deiodinase enzymes important in the activation and deactivation of thyroid hormones. Thyroxine (T4), the precursor of 3,5,3'-triiodothyronine (T3) is transformed into T3 by deiodinase activity. T3, through binding a nuclear thyroid hormone receptor, influences the expression of genes in practically every vertebrate cell. Iodothyronine deiodinases are unusual in that these enzymes contain selenium, in the form of an otherwise rare amino acid selenocysteine.
Thyroid-stimulating hormone (also known as thyrotropin, thyrotropic hormone, or abbreviated TSH) is a pituitary hormone that stimulates the thyroid gland to produce thyroxine (T4), and then triiodothyronine (T3) which stimulates the metabolism of almost every tissue in the body. It is a glycoprotein hormone produced by thyrotrope cells in the anterior pituitary gland, which regulates the endocrine function of the thyroid.

Thyroxine-binding globulin (TBG) is a globulin protein that in humans is encoded by the SERPINA7 gene. TBG binds thyroid hormones in circulation. It is one of three transport proteins (along with transthyretin and serum albumin) responsible for carrying the thyroid hormones thyroxine (T4) and triiodothyronine (T3) in the bloodstream. Of these three proteins, TBG has the highest affinity for T4 and T3 but is present in the lowest concentration relative to transthyretin and albumin, which also bind T3 and T4 in circulation. Despite its low concentration, TBG carries the majority of T4 in the blood plasma. Due to the very low concentration of T4 and T3 in the blood, TBG is rarely more than 25% saturated with its ligand. Unlike transthyretin and albumin, TBG has a single binding site for T4/T3. TBG is synthesized primarily in the liver as a 54-kDa protein. In terms of genomics, TBG is a serpin; however, it has no inhibitory function like many other members of this class of proteins.
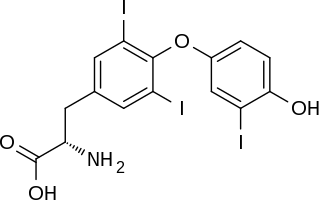
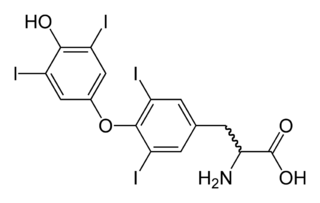
Triiodothyronine, also known as T3, is a thyroid hormone. It affects almost every physiological process in the body, including growth and development, metabolism, body temperature, and heart rate.

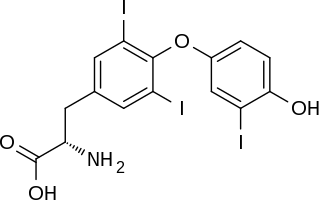
Levothyroxine, also known as L-thyroxine, is a synthetic form of the thyroid hormone thyroxine (T4). It is used to treat thyroid hormone deficiency (hypothyroidism), including a severe form known as myxedema coma. It may also be used to treat and prevent certain types of thyroid tumors. It is not indicated for weight loss. Levothyroxine is taken orally (by mouth) or given by intravenous injection. Levothyroxine has a half-life of 7.5 days when taken daily, so about six weeks is required for it to reach a steady level in the blood.
Thyroid disease is a medical condition that affects the function of the thyroid gland. The thyroid gland is located at the front of the neck and produces thyroid hormones that travel through the blood to help regulate many other organs, meaning that it is an endocrine organ. These hormones normally act in the body to regulate energy use, infant development, and childhood development.
Desiccated thyroid, also known as thyroid extract, is thyroid gland that has been dried and powdered for medical use. It is used to treat hypothyroidism. It is less preferred than levothyroxine. It is taken by mouth. Maximal effects may take up to three weeks to occur.

The hypothalamic–pituitary–thyroid axis is part of the neuroendocrine system responsible for the regulation of metabolism and also responds to stress.

Reverse triiodothyronine (3,3′,5′-triiodothyronine, reverse T3, or rT3) is an isomer of triiodothyronine (3,5,3′ triiodothyronine, T3).
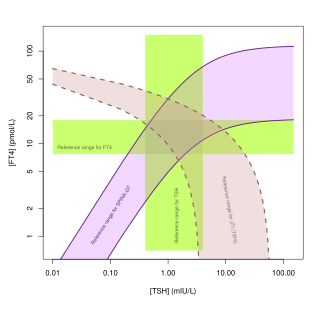
Euthyroid sick syndrome (ESS) is a state of adaptation or dysregulation of thyrotropic feedback control wherein the levels of T3 and/or T4 are abnormal, but the thyroid gland does not appear to be dysfunctional. This condition may result from allostatic responses of hypothalamus-pituitary-thyroid feedback control, dyshomeostatic disorders, drug interferences, and impaired assay characteristics in critical illness.
Myxedema coma is an extreme or decompensated form of hypothyroidism and while uncommon, is potentially lethal. A person may have laboratory values identical to a "normal" hypothyroid state, but a stressful event precipitates the myxedema coma state, usually in the elderly. Primary symptoms of myxedema coma are altered mental status and low body temperature. Low blood sugar, low blood pressure, hyponatremia, hypercapnia, hypoxia, slowed heart rate, and hypoventilation may also occur. Myxedema, although included in the name, is not necessarily seen in myxedema coma. Coma is also not necessarily seen in myxedema coma, as patients may be obtunded without being comatose.

Thyroid hormones are any hormones produced and released by the thyroid gland, namely triiodothyronine (T3) and thyroxine (T4). They are tyrosine-based hormones that are primarily responsible for regulation of metabolism. T3 and T4 are partially composed of iodine, derived from food. A deficiency of iodine leads to decreased production of T3 and T4, enlarges the thyroid tissue and will cause the disease known as simple goitre.
Thyroid disease in pregnancy can affect the health of the mother as well as the child before and after delivery. Thyroid disorders are prevalent in women of child-bearing age and for this reason commonly present as a pre-existing disease in pregnancy, or after childbirth. Uncorrected thyroid dysfunction in pregnancy has adverse effects on fetal and maternal well-being. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Due to an increase in thyroxine binding globulin, an increase in placental type 3 deioidinase and the placental transfer of maternal thyroxine to the fetus, the demand for thyroid hormones is increased during pregnancy. The necessary increase in thyroid hormone production is facilitated by high human chorionic gonadotropin (hCG) concentrations, which bind the TSH receptor and stimulate the maternal thyroid to increase maternal thyroid hormone concentrations by roughly 50%. If the necessary increase in thyroid function cannot be met, this may cause a previously unnoticed (mild) thyroid disorder to worsen and become evident as gestational thyroid disease. Currently, there is not enough evidence to suggest that screening for thyroid dysfunction is beneficial, especially since treatment thyroid hormone supplementation may come with a risk of overtreatment. After women give birth, about 5% develop postpartum thyroiditis which can occur up to nine months afterwards. This is characterized by a short period of hyperthyroidism followed by a period of hypothyroidism; 20–40% remain permanently hypothyroid.
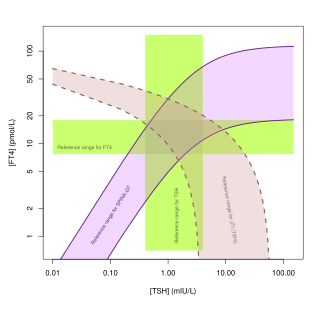
Thyroid's secretory capacity is the maximum stimulated amount of thyroxine that the thyroid can produce in a given time-unit.
The sum activity of peripheral deiodinases is the maximum amount of triiodothyronine produced per time-unit under conditions of substrate saturation. It is assumed to reflect the activity of deiodinases outside the central nervous system and other isolated compartments. GD is therefore expected to reflect predominantly the activity of type I deiodinase.
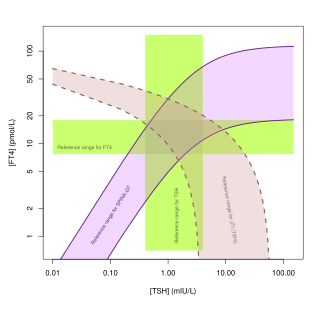
Jostel's TSH index, also referred to as Jostel's thyrotropin index or Thyroid Function index (TFI), is a method for estimating the thyrotropic function of the anterior pituitary lobe in a quantitative way. The equation has been derived from the logarithmic standard model of thyroid homeostasis. In a paper from 2014 further study was suggested to show if it is useful, but the 2018 guideline by the European Thyroid Association for the diagnosis of uncertain cases of central hypothyroidism regarded it as beneficial. It is also recommended for purposes of differential diagnosis in the sociomedical expert assessment.

SimThyr is a free continuous dynamic simulation program for the pituitary-thyroid feedback control system. The open-source program is based on a nonlinear model of thyroid homeostasis. In addition to simulations in the time domain the software supports various methods of sensitivity analysis. Its simulation engine is multi-threaded and supports multiple processor cores. SimThyr provides a GUI, which allows for visualising time series, modifying constant structure parameters of the feedback loop, storing parameter sets as XML files and exporting results of simulations in various formats that are suitable for statistical software. SimThyr is intended for both educational purposes and in-silico research.
The Thyrotroph Thyroid Hormone Sensitivity Index is a calculated structure parameter of thyroid homeostasis. It was originally developed to deliver a method for fast screening for resistance to thyroid hormone. Today it is also used to get an estimate for the set point of thyroid homeostasis, especially to assess dynamic thyrotropic adaptation of the anterior pituitary gland, including non-thyroidal illnesses.