Related Research Articles

Snoring is the vibration of respiratory structures and the resulting sound due to obstructed air movement during breathing while sleeping. The sound may be soft or loud and unpleasant. Snoring during sleep may be a sign, or first alarm, of obstructive sleep apnea (OSA). Research suggests that snoring is one of the factors of sleep deprivation.

Xylometazoline, also spelled xylomethazoline, is a medication used to reduce symptoms of nasal congestion, allergic rhinitis, and sinusitis. Use is not recommended for more than seven days. Use is also not recommended in those less than three months of age and some say not less than 6 years of age. It is used directly in the nose as a spray or drops.

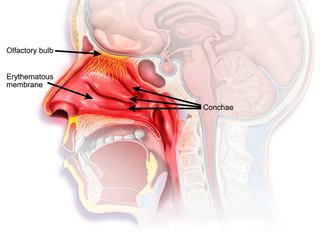
Allergic rhinitis, of which the seasonal type is called hay fever, is a type of inflammation in the nose that occurs when the immune system overreacts to allergens in the air. Signs and symptoms include a runny or stuffy nose, sneezing, red, itchy, and watery eyes, and swelling around the eyes. The fluid from the nose is usually clear. Symptom onset is often within minutes following allergen exposure, and can affect sleep and the ability to work or study. Some people may develop symptoms only during specific times of the year, often as a result of pollen exposure. Many people with allergic rhinitis also have asthma, allergic conjunctivitis, or atopic dermatitis.

Rhinitis, also known as coryza, is irritation and inflammation of the mucous membrane inside the nose. Common symptoms are a stuffy nose, runny nose, sneezing, and post-nasal drip.

Nasal polyps (NP) are noncancerous growths within the nose or sinuses. Symptoms include trouble breathing through the nose, loss of smell, decreased taste, post nasal drip, and a runny nose. The growths are sac-like, movable, and nontender, though face pain may occasionally occur. They typically occur in both nostrils in those who are affected. Complications may include sinusitis and broadening of the nose.
Upper airway resistance syndrome (UARS) is a sleep disorder characterized by the narrowing of the airway that can cause disruptions to sleep. The symptoms include unrefreshing sleep, fatigue, sleepiness, chronic insomnia, and difficulty concentrating. UARS can be diagnosed by polysomnograms capable of detecting Respiratory Effort-related Arousals. It can be treated with lifestyle changes, orthodontics, surgery, or CPAP therapy. UARS is considered a variant of sleep apnea, although some scientists and doctors believe it to be a distinct disorder.

Nasal sprays are used to deliver medications locally in the nasal cavities or systemically. They are used locally for conditions such as nasal congestion and allergic rhinitis. In some situations, the nasal delivery route is preferred for systemic therapy because it provides an agreeable alternative to injection or pills. Substances can be assimilated extremely quickly and directly through the nose. Many pharmaceutical drugs exist as nasal sprays for systemic administration. Other applications include hormone replacement therapy, treatment of Alzheimer's disease and Parkinson's disease. Nasal sprays are seen as a more efficient way of transporting drugs with potential use in crossing the blood–brain barrier.

Nasal septum deviation is a physical disorder of the nose, involving a displacement of the nasal septum. Some displacement is common, affecting 80% of people, mostly without their knowledge.
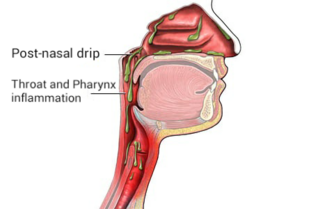
Post-nasal drip (PND), also known as upper airway cough syndrome (UACS), occurs when excessive mucus is produced by the nasal mucosa. The excess mucus accumulates in the back of the nose, and eventually in the throat once it drips down the back of the throat. It can be caused by rhinitis, sinusitis, gastroesophageal reflux disease (GERD), or by a disorder of swallowing. Other causes can be allergy, cold, flu, and side effects from medications.

Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is characterized by recurrent episodes of complete or partial obstruction of the upper airway leading to reduced or absent breathing during sleep. These episodes are termed "apneas" with complete or near-complete cessation of breathing, or "hypopneas" when the reduction in breathing is partial. In either case, a fall in blood oxygen saturation, a disruption in sleep, or both, may result. A high frequency of apneas or hypopneas during sleep may interfere with the quality of sleep, which – in combination with disturbances in blood oxygenation – is thought to contribute to negative consequences to health and quality of life. The terms obstructive sleep apnea syndrome (OSAS) or obstructive sleep apnea–hypopnea syndrome (OSAHS) may be used to refer to OSA when it is associated with symptoms during the daytime.

Rhinorrhea, rhinorrhoea, or informally runny nose is the free discharge of a thin mucus fluid from the nose; it is a common condition. It is a common symptom of allergies or certain viral infections, such as the common cold or COVID-19. It can be a side effect of crying, exposure to cold temperatures, cocaine abuse, or drug withdrawal, such as from methadone or other opioids. Treatment for rhinorrhea may be aimed at reducing symptoms or treating underlying causes. Rhinorrhea usually resolves without intervention, but may require treatment by a doctor if symptoms last more than 10 days or if symptoms are the result of foreign bodies in the nose.
Rhinitis medicamentosa is a condition of rebound nasal congestion suspected to be brought on by extended use of topical decongestants and certain oral medications that constrict blood vessels in the lining of the nose, although evidence has been contradictory.
Mouth breathing, medically known as chronic oral ventilation, is long-term breathing through the mouth. It often is caused by an obstruction to breathing through the nose, the innate breathing organ in the human body. Chronic mouth breathing may be associated with illness. The term "mouth-breather" has developed a pejorative slang meaning.

Empty nose syndrome (ENS) is a clinical syndrome, the hallmark symptom of which is a sensation of suffocation despite a clear airway. This syndrome is often referred to as a form of secondary atrophic rhinitis. ENS is a potential complication of nasal turbinate surgery or injury. Patients have usually undergone a turbinectomy or other surgical procedures that injure the nasal turbinates.
Chronic atrophic rhinitis, or simply atrophic rhinitis, is a chronic inflammation of the nose characterised by atrophy of nasal mucosa, including the glands, turbinate bones and the nerve elements supplying the nose. Chronic atrophic rhinitis may be primary and secondary. Special forms of chronic atrophic rhinitis are rhinitis sicca anterior and ozaena. It can also be described as the empty nose syndrome.

Continuous positive airway pressure (CPAP) is a form of positive airway pressure (PAP) ventilation in which a constant level of pressure greater than atmospheric pressure is continuously applied to the upper respiratory tract of a person. The application of positive pressure may be intended to prevent upper airway collapse, as occurs in obstructive sleep apnea, or to reduce the work of breathing in conditions such as acute decompensated heart failure. CPAP therapy is highly effective for managing obstructive sleep apnea. Compliance and acceptance of use of CPAP therapy can be a limiting factor, with 8% of people stopping use after the first night and 50% within the first year.

Adenoiditis is the inflammation of the adenoid tissue usually caused by an infection. Adenoiditis is treated using medication or surgical intervention.
Obligate nasal breathing describes a physiological instinct to breathe through the nose as opposed to breathing through the mouth.
Nasal expiratory positive airway pressure is a treatment for obstructive sleep apnea (OSA) and snoring.
Nonallergic rhinitis is rhinitis—inflammation of the inner part of the nose—not caused by an allergy. Nonallergic rhinitis displays symptoms including chronic sneezing or having a congested, drippy nose, without an identified allergic reaction. Other common terms for nonallergic rhinitis are vasomotor rhinitis and perennial rhinitis. The prevalence of nonallergic rhinitis in otolaryngology is 40%. Allergic rhinitis is more common than nonallergic rhinitis; however, both conditions have similar presentation, manifestation and treatment. Nasal itching and paroxysmal sneezing are usually associated with nonallergic rhinitis rather than allergic rhinitis.
References
- ↑ "Nasal congestion". MedlinePlus Medical Encyclopedia. A.D.A.M., Inc.
- ↑ Rao A, ed. (2012). Principles and Practice of Pedodontics (3rd ed.). New Delhi: Jaypee Brothers Medical Pub. pp. 169, 170. ISBN 9789350258910.
- ↑ Turowski, Jason (2016-04-29). "Should You Breathe Through Your Mouth or Your Nose?". Cleveland Clinic . Retrieved 2020-06-28.
- ↑ Bergeson PS, Shaw JC (October 2001). "Are infants really obligatory nasal breathers?". Clinical Pediatrics. 40 (10): 567–9. doi:10.1177/000992280104001006. PMID 11681824. S2CID 44715721.
- ↑ de Oliveira, Pedro Wey Barbosa; Gregorio, Luciano Lobato; Silva, Rogério Santos; Bittencourt, Lia Rita Azevedo; Tufik, Sergio; Gregório, Luis Carlos (July 2016). "Orofacial-cervical alterations in individuals with upper airway resistance syndrome". Brazilian Journal of Otorhinolaryngology. 82 (4): 377–384. doi: 10.1016/j.bjorl.2015.05.015 . PMC 9448996 . PMID 26671020.
- ↑ Buschang PH, Carrillo R, Rossouw PE (March 2011). "Orthopedic correction of growing hyperdivergent, retrognathic patients with miniscrew implants". Journal of Oral and Maxillofacial Surgery. 69 (3): 754–62. doi:10.1016/j.joms.2010.11.013. PMC 3046301 . PMID 21236539.
- 1 2 3 4 5 6 7 Nasal congestion at MedlinePlus, a service of the U.S. National Library of Medicine, National Institutes of Health. Update Date: 8/2/2011. Updated by: Neil K. Kaneshiro. Also reviewed by David Zieve.
- ↑ "Blocked Nose, Restricted Air Flow". Aerin Medical. Archived from the original on 2016-08-26. Retrieved 2016-07-12.
- ↑ Pacheco-Galván A, Hart SP, Morice AH (April 2011). "Relationship between gastro-oesophageal reflux and airway diseases: the airway reflux paradigm". Archivos de Bronconeumologia. 47 (4): 195–203. doi:10.1016/j.arbres.2011.02.001. PMID 21459504.
- ↑ Wang DY, Raza MT, Gordon BR (June 2004). "Control of nasal obstruction in perennial allergic rhinitis". Current Opinion in Allergy and Clinical Immunology. 4 (3): 165–70. doi:10.1097/00130832-200406000-00005. PMID 15126936. S2CID 20608574.
- ↑ Wang DY, Raza MT, Goh DY, Lee BW, Chan YH (July 2004). "Acoustic rhinometry in nasal allergen challenge study: which dimensional measures are meaningful?". Clinical and Experimental Allergy. 34 (7): 1093–8. doi:10.1111/j.1365-2222.2004.01988.x. PMID 15248855. S2CID 28523614.
- ↑ Šidlauskienė M, Smailienė D, Lopatienė K, Čekanauskas E, Pribuišienė R, Šidlauskas M (June 2015). "Relationships between Malocclusion, Body Posture, and Nasopharyngeal Pathology in Pre-Orthodontic Children". Medical Science Monitor. 21: 1765–73. doi:10.12659/MSM.893395. PMC 4484615 . PMID 26086193.
- ↑ Swiner, Carmelita (2020-01-27). "'How to Treat Nasal Congestion and Sinus Pressure". WebMD. Retrieved 2020-06-28.
- ↑ Nair, Satish (2011-04-12). "Nasal Breathing Exercise and its Effect on Symptoms of Allergic Rhinitis". Indian Journal of Otolaryngology and Head and Neck Surgery. Indian J Otolaryngol Head Neck Surg. 64 (2): 172–176. doi:10.1007/s12070-011-0243-5. PMC 3392338 . PMID 23730580.
- ↑ "Is Your Nose Working Against You? 5 Signs of a Deviated Septum". Cleveland Clinic. 7 November 2019. Retrieved 2020-06-28.