Related Research Articles
Spasticity is a feature of altered skeletal muscle performance with a combination of paralysis, increased tendon reflex activity, and hypertonia. It is also colloquially referred to as an unusual "tightness", stiffness, or "pull" of muscles.
Hereditary spastic paraplegia (HSP) is a group of inherited diseases whose main feature is a progressive gait disorder. The disease presents with progressive stiffness (spasticity) and contraction in the lower limbs. HSP is also known as hereditary spastic paraparesis, familial spastic paraplegia, French settlement disease, Strumpell disease, or Strumpell-Lorrain disease. The symptoms are a result of dysfunction of long axons in the spinal cord. The affected cells are the primary motor neurons; therefore, the disease is an upper motor neuron disease. HSP is not a form of cerebral palsy even though it physically may appear and behave much the same as spastic diplegia. The origin of HSP is different from cerebral palsy. Despite this, some of the same anti-spasticity medications used in spastic cerebral palsy are sometimes used to treat HSP symptoms.

The pyramidal tracts include both the corticobulbar tract and the corticospinal tract. These are aggregations of efferent nerve fibers from the upper motor neurons that travel from the cerebral cortex and terminate either in the brainstem (corticobulbar) or spinal cord (corticospinal) and are involved in the control of motor functions of the body.
Clonus is a set of involuntary and rhythmic muscular contractions and relaxations. Clonus is a sign of certain neurological conditions, particularly associated with upper motor neuron lesions involving descending motor pathways, and in many cases is, accompanied by spasticity. Unlike small, spontaneous twitches known as fasciculations, clonus causes large motions that are usually initiated by a reflex. Studies have shown clonus beat frequency to range from three to eight Hz on average, and may last a few seconds to several minutes depending on the patient’s condition. The term is from the Greek for "violent, confused motion"

Functional electrical stimulation (FES) is a technique that uses low-energy electrical pulses to artificially generate body movements in individuals who have been paralyzed due to injury to the central nervous system. More specifically, FES can be used to generate muscle contraction in otherwise paralyzed limbs to produce functions such as grasping, walking, bladder voiding and standing. This technology was originally used to develop neuroprostheses that were implemented to permanently substitute impaired functions in individuals with spinal cord injury (SCI), head injury, stroke and other neurological disorders. In other words, a person would use the device each time he or she wanted to generate a desired function. FES is sometimes also referred to as neuromuscular electrical stimulation (NMES).
A gait is a pattern of limb movements made during locomotion. Human gaits are the various ways in which a human can move, either naturally or as a result of specialized training. Human gait is defined as bipedal, biphasic forward propulsion of the center of gravity of the human body, in which there are alternate sinuous movements of different segments of the body with least expenditure of energy. Different gait patterns are characterized by differences in limb-movement patterns, overall velocity, forces, kinetic and potential energy cycles, and changes in the contact with the ground.
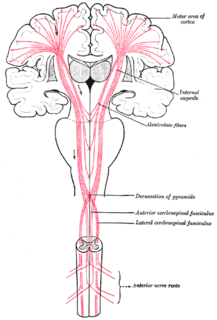
An upper motor neuron lesion occurs in the neural pathway above the anterior horn cell of the spinal cord or motor nuclei of the cranial nerves. Conversely, a lower motor neuron lesion affects nerve fibers traveling from the anterior horn of the spinal cord or the cranial motor nuclei to the relevant muscle(s).
The rectus femoris muscle is one of the four quadriceps muscles of the human body. The others are the vastus medialis, the vastus intermedius, and the vastus lateralis. All four parts of the quadriceps muscle attach to the patella by the quadriceps tendon.
Hypertonia is a term sometimes used synonymously with spasticity and rigidity in the literature surrounding damage to the central nervous system, namely upper motor neuron lesions. Impaired ability of damaged motor neurons to regulate descending pathways gives rise to disordered spinal reflexes, increased excitability of muscle spindles, and decreased synaptic inhibition. These consequences result in abnormally increased muscle tone of symptomatic muscles. Some authors suggest that the current definition for spasticity, the velocity-dependent over-activity of the stretch reflex, is not sufficient as it fails to take into account patients exhibiting increased muscle tone in the absence of stretch reflex over-activity. They instead suggest that "reversible hypertonia" is more appropriate and represents a treatable condition that is responsive to various therapy modalities like drug and/or physical therapy.

Foot drop is a gait abnormality in which the dropping of the forefoot happens due to weakness, irritation or damage to the deep fibular nerve, including the sciatic nerve, or paralysis of the muscles in the anterior portion of the lower leg. It is usually a symptom of a greater problem, not a disease in itself. Foot drop is characterized by inability or impaired ability to raise the toes or raise the foot from the ankle (dorsiflexion). Foot drop may be temporary or permanent, depending on the extent of muscle weakness or paralysis and it can occur in one or both feet. In walking, the raised leg is slightly bent at the knee to prevent the foot from dragging along the ground.
In medicine, physiotherapy, chiropractic, and osteopathy the hip examination, or hip exam, is undertaken when a patient has a complaint of hip pain and/or signs and/or symptoms suggestive of hip joint pathology. It is a physical examination maneuver.
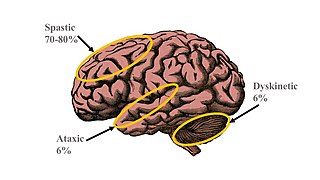
Spastic diplegia, is a form of cerebral palsy (CP) that is a chronic neuromuscular condition of hypertonia and spasticity—manifested as an especially high and constant "tightness" or "stiffness"—in the muscles of the lower extremities of the human body, usually those of the legs, hips and pelvis. Doctor William John Little's first recorded encounter with cerebral palsy is reported to have been among children who displayed signs of spastic diplegia.
Diplegia, when used singularly, refers to paralysis affecting symmetrical parts of the body. This is different from hemiplegia which refers to spasticity restricted to one side of the body, paraplegia which refers to paralysis restricted to the legs and hip, and quadriplegia which requires the involvement of all four limbs but not necessarily symmetrical. Diplegia is the most common cause of crippling in children, specifically in children with cerebral palsy. Other causes may be due to injury of the spinal cord. There is no set course of progression for people with diplegia. Symptoms may get worse but the neurological part does not change. The primary parts of the brain that are affected by diplegia are the ventricles, fluid filled compartments in the brain, and the wiring from the center of the brain to the cerebral cortex. There is also usually some degeneration of the cerebral neurons, as well as problems in the upper motor neuron system. The term diplegia can refer to any bodily area, such as the face, arms, or legs.
A selective dorsal rhizotomy (SDR), also known as a rhizotomy, dorsal rhizotomy, or a selective posterior rhizotomy, is a neurosurgical procedure that selectively destroys problematic nerve roots in the spinal cord. This procedure has been well-established in the literature as a surgical intervention and is used to relieve negative symptoms of neuromuscular conditions such as spastic diplegia and other forms of spastic cerebral palsy. The specific sensory nerves inducing spasticity are identified using electromyographic (EMG) stimulation and graded on a scale of 1 (mild) to 4. Abnormal nerve responses are isolated and cut, thereby reducing symptoms of spasticity.
Spastic quadriplegia, also known as spastic tetraplegia, is a subset of spastic cerebral palsy that affects all four limbs.

Orthotics is a medical specialty that focuses on the design and application of orthoses. An orthosis is "an externally applied device used to influence the structural and functional characteristics of the neuromuscular and skeletal system".

Over time, the approach to cerebral palsy management has shifted away from narrow attempts to fix individual physical problems – such as spasticity in a particular limb – to making such treatments part of a larger goal of maximizing the person's independence and community engagement. Much of childhood therapy is aimed at improving gait and walking. Approximately 60% of people with CP are able to walk independently or with aids at adulthood. However, the evidence base for the effectiveness of intervention programs reflecting the philosophy of independence has not yet caught up: effective interventions for body structures and functions have a strong evidence base, but evidence is lacking for effective interventions targeted toward participation, environment, or personal factors. There is also no good evidence to show that an intervention that is effective at the body-specific level will result in an improvement at the activity level, or vice versa. Although such cross-over benefit might happen, not enough high-quality studies have been done to demonstrate it.
Upper motor neuron syndrome (UMNS) is the motor control changes that can occur in skeletal muscle after an upper motor neuron lesion.

Spastic cerebral palsy is the type of cerebral palsy characterized by spasticity or high muscle tone often resulting in stiff, jerky movements. Cases of spastic CP are further classified according to the part or parts of the body that are most affected. Such classifications include spastic diplegia, spastic hemiplegia, spastic quadriplegia, and in cases of single limb involvement, spastic monoplegia.

Spastic hemiplegia is a neuromuscular condition of spasticity that results in the muscles on one side of the body being in a constant state of contraction. It is the "one-sided version" of spastic diplegia. It falls under the mobility impairment umbrella of cerebral palsy. About 20–30% of people with cerebral palsy have spastic hemiplegia. Due to brain or nerve damage, the brain is constantly sending action potentials to the neuromuscular junctions on the affected side of the body. Similar to strokes, damage on the left side of the brain affects the right side of the body and damage on the right side of the brain affects the left side of the body. Other side can be effected for lesser extent. The affected side of the body is rigid, weak and has low functional abilities. In most cases, the upper extremity is much more affected than the lower extremity. This could be due to preference of hand usage during early development. If both arms are affected, the condition is referred to as double hemiplegia. Some patients with spastic hemiplegia only suffer minor impairments, where in severe cases one side of the body could be completely paralyzed. The severity of spastic hemiplegia is dependent upon the degree of the brain or nerve damage.
References
- ↑ Saint, Sanjay; Wiese, Jeff; Bent, Stephen (2006). Clinical clerkships: the answer book. Hagerstown, MD: Lippincott Williams & Wilkins. p. 219. ISBN 0-7817-3754-0.
- ↑ Medline Plus
- ↑ GP Notebook