Temporomandibular joint dysfunction is an umbrella term covering pain and dysfunction of the muscles of mastication and the temporomandibular joints. The most important feature is pain, followed by restricted mandibular movement, and noises from the temporomandibular joints (TMJ) during jaw movement. Although TMD is not life-threatening, it can be detrimental to quality of life; this is because the symptoms can become chronic and difficult to manage.

Tetanus, also known as lockjaw, is a bacterial infection caused by Clostridium tetani and characterized by muscle spasms. In the most common type, the spasms begin in the jaw, and then progress to the rest of the body. Each spasm usually lasts for a few minutes. Spasms occur frequently for three to four weeks. Some spasms may be severe enough to fracture bones. Other symptoms of tetanus may include fever, sweating, headache, trouble swallowing, high blood pressure, and a fast heart rate. Onset of symptoms is typically 3 to 21 days following infection. Recovery may take months; about 10% of cases prove to be fatal.
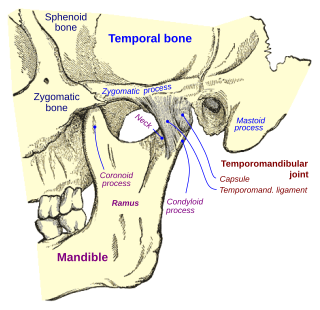
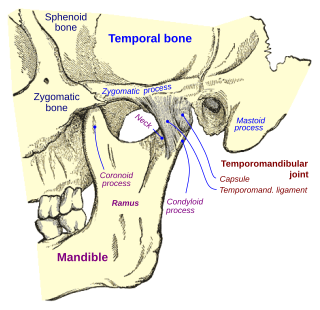
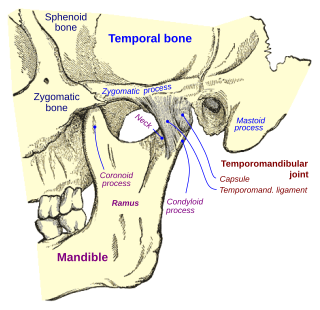
In anatomy, the temporomandibular joints (TMJ) are the two joints connecting the jawbone to the skull. It is a bilateral synovial articulation between the temporal bone of the skull above and the mandible below; it is from these bones that its name is derived. The joints are unique in their bilateral function, being connected via the mandible.

Peritonsillar abscess (PTA), also known as quinsy, is an accumulation of pus due to an infection behind the tonsil. Symptoms include fever, throat pain, trouble opening the mouth, and a change to the voice. Pain is usually worse on one side. Complications may include blockage of the airway or aspiration pneumonitis.

Pericoronitis is inflammation of the soft tissues surrounding the crown of a partially erupted tooth, including the gingiva (gums) and the dental follicle. The soft tissue covering a partially erupted tooth is known as an operculum, an area which can be difficult to access with normal oral hygiene methods. The hyponym operculitis technically refers to inflammation of the operculum alone.

Meige's syndrome is a type of dystonia. It is also known as Brueghel's syndrome and oral facial dystonia. It is actually a combination of two forms of dystonia, blepharospasm and oromandibular dystonia (OMD).

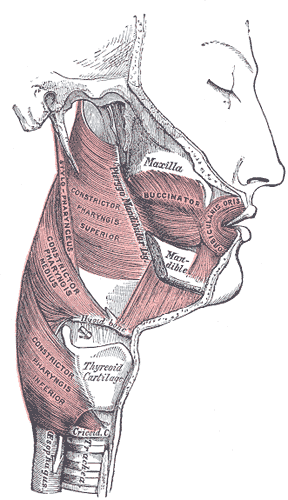
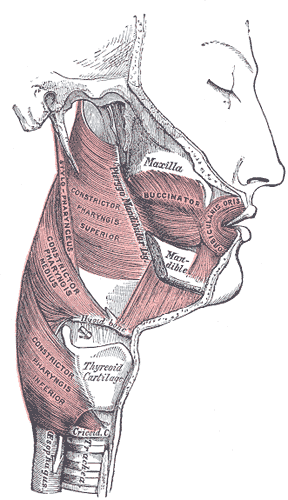
Masticatory muscle myositis (MMM) is an inflammatory disease in dogs affecting the muscles of mastication (chewing). It is also known as atrophic myositis or eosinophilic myositis. MMM is the most common inflammatory myopathy in dogs. The disease mainly affects large breed dogs. German Shepherd Dogs and Cavalier King Charles Spaniels may be predisposed. There is a similar disease of the eye muscles found in Golden Retrievers. Symptoms of acute MMM include swelling of the jaw muscles, drooling, and pain on opening the mouth. Ophthalmic signs may include third eyelid protrusion, red eyes, and exophthalmos. In chronic MMM there is atrophy of the jaw muscles, and scarring of the masticatory muscles due to fibrosis may result in inability to open the mouth (trismus). The affected muscles include the temporalis, masseter, and pterygoid muscles. The disease is usually bilateral.
A dental emergency is an issue involving the teeth and supporting tissues that are of high importance to be treated by the relevant professional. Dental emergencies do not always involve pain, although this is a common signal that something needs to be looked at. Pain can originate from the tooth, surrounding tissues or can have the sensation of originating in the teeth but be caused by an independent source. Depending on the type of pain experienced an experienced clinician can determine the likely cause and can treat the issue as each tissue type gives different messages in a dental emergency.
The buccal space is a fascial space of the head and neck. It is a potential space in the cheek, and is paired on each side. The buccal space is superficial to the buccinator muscle and deep to the platysma muscle and the skin. The buccal space is part of the subcutaneous space, which is continuous from head to toe.
Mouth infections, also known as oral infections, are a group of infections that occur around the oral cavity. They include dental infection, dental abscess, and Ludwig's angina. Mouth infections typically originate from dental caries at the root of molars and premolars that spread to adjacent structures. In otherwise healthy patients, removing the offending tooth to allow drainage will usually resolve the infection. In cases that spread to adjacent structures or in immunocompromised patients, surgical drainage and systemic antibiotics may be required in addition to tooth extraction. Since bacteria that normally reside in the oral cavity cause mouth infections, proper dental hygiene can prevent most cases of infection. As such, mouth infections are more common in populations with poor access to dental care or populations with health-related behaviors that damage one's teeth and oral mucosa. This is a common problem, representing nearly 36% of all encounters within the emergency department related to dental conditions.
Oral submucous fibrosis (OSF) is a chronic, complex, premalignant condition of the oral cavity, characterized by juxta-epithelial inflammatory reaction and progressive fibrosis of the submucosal tissues. As the disease progresses, the oral mucosa becomes fibrotic to the point that the person is unable to open the mouth. The condition is remotely linked to oral cancers and is associated with the chewing of areca nut and/or its byproducts, commonly practiced in South and South-East Asian countries. The incidence of OSF has also increased in western countries due to changing habits and population migration.
Fibrous ankylosis is a condition that affects fibrous connective tissue causing a limited range of movement.
Dentomandibular sensorimotor dysfunction (DMSD) is a medical condition involving the mandible, upper three cervical (neck) vertebrae, and the surrounding muscle and nerve areas.
Fascial spaces are potential spaces that exist between the fasciae and underlying organs and other tissues. In health, these spaces do not exist; they are only created by pathology, e.g. the spread of pus or cellulitis in an infection. The fascial spaces can also be opened during the dissection of a cadaver. The fascial spaces are different from the fasciae themselves, which are bands of connective tissue that surround structures, e.g. muscles. The opening of fascial spaces may be facilitated by pathogenic bacterial release of enzymes which cause tissue lysis. The spaces filled with loose areolar connective tissue may also be termed clefts. Other contents such as salivary glands, blood vessels, nerves and lymph nodes are dependent upon the location of the space. Those containing neurovascular tissue may also be termed compartments.

The submasseterric space is a fascial space of the head and neck. It is a potential space in the face over the angle of the jaw, and is paired on each side. It is located between the lateral aspect of the mandible and the medial aspect of the masseter muscle and its investing fascia. The term is derived from sub- meaning "under" in Latin and masseteric which refers to the masseter muscle. The submasseteric space is one of the four compartments of the masticator space. Sometimes the submasseteric space is described as a series of spaces, created because the masseter muscle has multiple insertions that cover most of the lateral surface of the ramus of the mandible.
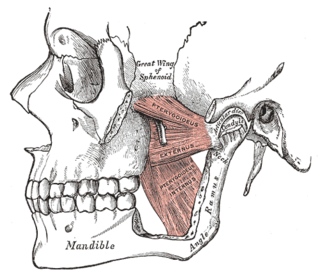
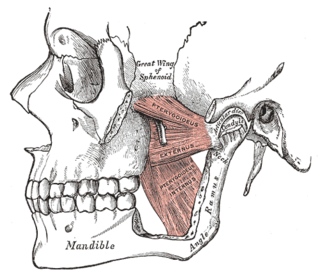
The pterygomandibular space is a fascial space of the head and neck. It is a potential space in the head and is paired on each side. It is located between the lateral pterygoid muscle and the medial surface of the ramus of the mandible. The pterygomandibular space is one of the four compartments of the masticator space.

The infratemporal space is a fascial space of the head and neck. It is a potential space in the side of the head, and is paired on either side. It is located posterior to the maxilla, between the lateral pterygoid plate of the sphenoid bone medially and by the base of skull superiorly. The term is derived from infra- meaning below and temporal which refers to the temporalis muscle.
Osteomyelitis of the jaws is osteomyelitis which occurs in the bones of the jaws. Historically, osteomyelitis of the jaws was a common complication of odontogenic infection. Before the antibiotic era, it was frequently a fatal condition.
A parapharyngeal abscess is a deep neck space abscess of the parapharyngeal space, which is lateral to the superior pharyngeal constrictor muscle and medial to the masseter muscle. This space is divided by the styloid process into anterior and posterior compartments. The posterior compartment contains the carotid artery, internal jugular vein, and many nerves.