The salivary glands in many vertebrates including mammals are exocrine glands that produce saliva through a system of ducts. Humans have three paired major salivary glands, as well as hundreds of minor salivary glands. Salivary glands can be classified as serous, mucous, or seromucous (mixed).

A thyroglossal cyst is a fibrous cyst that forms from a persistent thyroglossal duct. Thyroglossal cysts can be defined as an irregular neck mass or a lump which develops from cells and tissues left over after the formation of the thyroid gland during developmental stages.
The oral mucosa is the mucous membrane lining the inside of the mouth. It comprises stratified squamous epithelium, termed "oral epithelium", and an underlying connective tissue termed lamina propria. The oral cavity has sometimes been described as a mirror that reflects the health of the individual. Changes indicative of disease are seen as alterations in the oral mucosa lining the mouth, which can reveal systemic conditions, such as diabetes or vitamin deficiency, or the local effects of chronic tobacco or alcohol use. The oral mucosa tends to heal faster and with less scar formation compared to the skin. The underlying mechanism remains unknown, but research suggests that extracellular vesicles might be involved.

Fordyce spots are harmless and painless visible sebaceous glands typically appearing as white/yellow small bumps or spots on the inside of lips or cheeks, gums, or genitalia. They are common, and are present in around 80% of adults. Treatment is generally not required and attempts to remove them typically result in pain and scarring.

A ranula is a mucus extravasation cyst involving a sublingual gland and is a type of mucocele found on the floor of the mouth. Ranulae present as a swelling of connective tissue consisting of collected mucin from a ruptured salivary gland caused by local trauma. If small and asymptomatic further treatment may not be needed, otherwise minor oral surgery may be indicated.
Inflammatory papillary hyperplasia (IPH) is a benign lesion of the oral mucosa which is characterized by the growth of one or more nodular lesions, measuring about 2mm or less. The lesion almost exclusively involves the hard palate, and in rare instances, it also has been seen on the mandible. The lesion is mostly asymptomatic and color of the mucosa may vary from pink to red.
An oral medicine or stomatology doctor/dentist has received additional specialized training and experience in the diagnosis and management of oral mucosal abnormalities including oral cancer, salivary gland disorders, temporomandibular disorders and facial pain, taste and smell disorders; and recognition of the oral manifestations of systemic and infectious diseases. It lies at the interface between medicine and dentistry. An oral medicine doctor is trained to diagnose and manage patients with disorders of the orofacial region.

Sialadenitis (sialoadenitis) is inflammation of salivary glands, usually the major ones, the most common being the parotid gland, followed by submandibular and sublingual glands. It should not be confused with sialadenosis (sialosis) which is a non-inflammatory enlargement of the major salivary glands.

Acinic cell carcinoma is a malignant tumor representing 2% of all salivary tumors. 90% of the time found in the parotid gland, 10% intraorally on buccal mucosa or palate. The disease presents as a slow growing mass, associated with pain or tenderness in 50% of the cases. Often appears pseudoencapsulated.

Salivary gland tumours, also known as mucous gland adenomas or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.
Dental pertains to the teeth, including dentistry. Topics related to the dentistry, the human mouth and teeth include:
Oral and maxillofacial pathology refers to the diseases of the mouth, jaws and related structures such as salivary glands, temporomandibular joints, facial muscles and perioral skin. The mouth is an important organ with many different functions. It is also prone to a variety of medical and dental disorders.
Oral pigmentation is asymptomatic and does not usually cause any alteration to the texture or thickness of the affected area. The colour can be uniform or speckled and can appear solitary or as multiple lesions. Depending on the site, depth, and quantity of pigment, the appearance can vary considerably.
A mucocele is a distension of a hollow organ or cavity because of mucus buildup.
Odontogenic cyst are a group of jaw cysts that are formed from tissues involved in odontogenesis. Odontogenic cysts are closed sacs, and have a distinct membrane derived from rests of odontogenic epithelium. It may contain air, fluids, or semi-solid material. Intra-bony cysts are most common in the jaws, because the mandible and maxilla are the only bones with epithelial components. That odontogenic epithelium is critical in normal tooth development. However, epithelial rests may be the origin for the cyst lining later. Not all oral cysts are odontogenic cysts. For example, mucous cyst of the oral mucosa and nasolabial duct cyst are not of odontogenic origin.

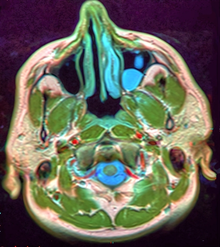
Salivary gland diseases (SGDs) are multiple and varied in cause. There are three paired major salivary glands in humans: the parotid glands, the submandibular glands, and the sublingual glands. There are also about 800–1,000 minor salivary glands in the mucosa of the mouth. The parotid glands are in front of the ears, one on side, and secrete mostly serous saliva, via the parotid ducts, into the mouth, usually opening roughly opposite the second upper molars. The submandibular gland is medial to the angle of the mandible, and it drains its mixture of serous and mucous saliva via the submandibular duct into the mouth, usually opening in a punctum in the floor of mouth. The sublingual gland is below the tongue, on the floor of the mouth; it drains its mostly mucous saliva into the mouth via about 8–20 ducts, which open along the plica sublingualis, a fold of tissue under the tongue.
Basal cell adenoma is a rare, low-grade benign salivary gland neoplasm.

Oroantral fistula (OAF) is an epithelialised oroantral communication (OAC). OAC refers to an abnormal connection between the oral cavity and antrum. The creation of an OAC is most commonly due to the extraction of a maxillary (upper) tooth closely related to the antral floor. A small OAC may heal spontaneously but a larger OAC would require surgical closure to prevent the development of persistent OAF and chronic sinusitis.

Gingival cyst, also known as Epstein's pearl, is a type of cysts of the jaws that originates from the dental lamina and is found in the mouth parts. It is a superficial cyst in the alveolar mucosa. It can be seen inside the mouth as small and whitish bulge. Depending on the ages in which they develop, the cysts are classified into gingival cyst of newborn and gingival cyst of adult. Structurally, the cyst is lined by thin epithelium and shows a lumen usually filled with desquamated keratin, occasionally containing inflammatory cells. The nodes are formed as a result of cystic degeneration of epithelial rests of the dental lamina.
Periapical granuloma, also sometimes referred to as a radicular granuloma or apical granuloma, is an inflammation at the tip of a dead (nonvital) tooth. It is a lesion or mass that typically starts out as an epithelial lined cyst, and undergoes an inward curvature that results in inflammation of granulation tissue at the root tips of a dead tooth. This is usually due to dental caries or a bacterial infection of the dental pulp. Periapical granuloma is an infrequent disorder that has an occurrence rate between 9.3 to 87.1 percent. Periapical granuloma is not a true granuloma due to the fact that it does not contain granulomatous inflammation; however, periapical granuloma is a common term used.