A cleanroom or clean room is an engineered space that maintains a very low concentration of airborne particulates. It is well isolated, well controlled from contamination, and actively cleansed. Such rooms are commonly needed for scientific research and in industrial production for all nanoscale processes, such as semiconductor manufacturing. A cleanroom is designed to keep everything from dust to airborne organisms or vaporised particles away from it, and so from whatever material is being handled inside it.

Sterilization refers to any process that removes, kills, or deactivates all forms of life and other biological agents present in fluid or on a specific surface or object. Sterilization can be achieved through various means, including heat, chemicals, irradiation, high pressure, and filtration. Sterilization is distinct from disinfection, sanitization, and pasteurization, in that those methods reduce rather than eliminate all forms of life and biological agents present. After sterilization, fluid or an object is referred to as being sterile or aseptic.
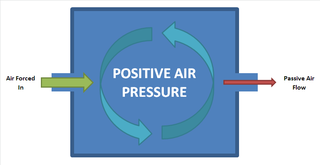
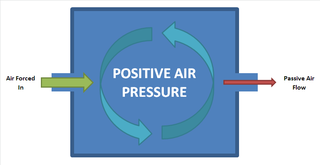
Positive pressure is a pressure within a system that is greater than the environment that surrounds that system. Consequently, if there is any leak from the positively pressured system, it will egress into the surrounding environment. This is in contrast to a negative pressure room, where air is sucked in.

HEPA filter, also known as a high efficiency particulate arresting filter, is an efficiency standard of air filters.
In medicine, public health, and biology, transmission is the passing of a pathogen causing communicable disease from an infected host individual or group to a particular individual or group, regardless of whether the other individual was previously infected. The term strictly refers to the transmission of microorganisms directly from one individual to another by one or more of the following means:

A hospital-acquired infection, also known as a nosocomial infection, is an infection that is acquired in a hospital or other healthcare facility. To emphasize both hospital and nonhospital settings, it is sometimes instead called a healthcare-associated infection. Such an infection can be acquired in a hospital, nursing home, rehabilitation facility, outpatient clinic, diagnostic laboratory or other clinical settings. A number of dynamic processes can bring contamination into operating rooms and other areas within nosocomial settings. Infection is spread to the susceptible patient in the clinical setting by various means. Healthcare staff also spread infection, in addition to contaminated equipment, bed linens, or air droplets. The infection can originate from the outside environment, another infected patient, staff that may be infected, or in some cases, the source of the infection cannot be determined. In some cases the microorganism originates from the patient's own skin microbiota, becoming opportunistic after surgery or other procedures that compromise the protective skin barrier. Though the patient may have contracted the infection from their own skin, the infection is still considered nosocomial since it develops in the health care setting. The term nosocomial infection is used when there is a lack of evidence that the infection was present when the patient entered the healthcare setting, thus meaning it was acquired or became problematic post-admission.
An antimicrobial is an agent that kills microorganisms (microbicide) or stops their growth. Antimicrobial medicines can be grouped according to the microorganisms they act primarily against. For example, antibiotics are used against bacteria, and antifungals are used against fungi. They can also be classified according to their function. The use of antimicrobial medicines to treat infection is known as antimicrobial chemotherapy, while the use of antimicrobial medicines to prevent infection is known as antimicrobial prophylaxis.
An air purifier or air cleaner is a device which removes contaminants from the air in a room to improve indoor air quality. These devices are commonly marketed as being beneficial to allergy sufferers and asthmatics, and at reducing or eliminating second-hand tobacco smoke.
Infection prevention and control is the discipline concerned with preventing healthcare-associated infections; a practical rather than academic sub-discipline of epidemiology. In Northern Europe, infection prevention and control is expanded from healthcare into a component in public health, known as "infection protection". It is an essential part of the infrastructure of health care. Infection control and hospital epidemiology are akin to public health practice, practiced within the confines of a particular health-care delivery system rather than directed at society as a whole.

Ultraviolet germicidal irradiation (UVGI) is a disinfection technique employing ultraviolet (UV) light, particularly UV-C (180–280 nm), to kill or inactivate microorganisms. UVGI primarily inactivates microbes by damaging their genetic material, thereby inhibiting their capacity to carry out vital functions.

Bioaerosols are a subcategory of particles released from terrestrial and marine ecosystems into the atmosphere. They consist of both living and non-living components, such as fungi, pollen, bacteria and viruses. Common sources of bioaerosols include soil, water, and sewage.

In health care facilities, isolation represents one of several measures that can be taken to implement in infection control: the prevention of communicable diseases from being transmitted from a patient to other patients, health care workers, and visitors, or from outsiders to a particular patient. Various forms of isolation exist, in some of which contact procedures are modified, and others in which the patient is kept away from all other people. In a system devised, and periodically revised, by the U.S. Centers for Disease Control and Prevention (CDC), various levels of patient isolation comprise application of one or more formally described "precaution".
Vaporized hydrogen peroxide (trademarked VHP, also known as hydrogen peroxide vapor, HPV) is a vapor form of hydrogen peroxide (H2O2) with applications as a low-temperature antimicrobial vapor used to decontaminate enclosed and sealed areas such as laboratory workstations, isolation and pass-through rooms, and even aircraft interiors.

Airborne transmission or aerosol transmission is transmission of an infectious disease through small particles suspended in the air. Infectious diseases capable of airborne transmission include many of considerable importance both in human and veterinary medicine. The relevant infectious agent may be viruses, bacteria, or fungi, and they may be spread through breathing, talking, coughing, sneezing, raising of dust, spraying of liquids, flushing toilets, or any activities which generate aerosol particles or droplets.
Indoor bioaerosol is bioaerosol in an indoor environment. Bioaerosols are natural or artificial particles of biological origin suspended in the air. These particles are also referred to as organic dust. Bioaerosols may consist of bacteria, fungi, viruses, microbial toxins, pollen, plant fibers, etc. Size of bioaerosol particles varies from below 1 μm to 100 μm in aerodynamic diameter; viable bioaerosol particles can be suspended in air as single cells or aggregates of microorganism as small as 1–10 μm in size. Since bioaerosols are potentially related to various human health effects and the indoor environment provides a unique exposure situation, concerns about indoor bioaerosols have increased over the last decade.

Negative room pressure is an isolation technique used in hospitals and medical centers to prevent cross-contamination from room to room. It includes a ventilation that generates negative pressure to allow air to flow into the isolation room but not escape from the room, as air will naturally flow from areas with higher pressure to areas with lower pressure, thereby preventing contaminated air from escaping the room. This technique is used to isolate patients with airborne contagious diseases such as: influenza (flu), measles, chickenpox, tuberculosis (TB), severe acute respiratory syndrome (SARS-CoV), Middle East respiratory syndrome (MERS-CoV), and coronavirus disease 2019 (COVID-19).
Bioburden is normally defined as the number of bacteria living on a surface that has not been sterilized.
Air filtration guidelines for operating rooms are determined by the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) using a standard known as Minimum Efficiency Reporting Value (MERV). MERV is determined based on the size of particles successfully removed from the air and is used to classify the efficiency of HEPA filters. Ratings range from 1-16 and efficiency increases as the rating increases. ASHRAE groups surgeries into three categories: minor surgical procedures (A); minor or major surgical procedures performed with minor sedation (B); and major surgical procedures performed with general anesthesia or regional block anesthesia (C). Each surgical category is given a minimum MERV rating it must comply with.

Source control is a strategy for reducing disease transmission by blocking respiratory secretions produced through breathing, speaking, coughing, sneezing or singing. Multiple source control techniques can be used in hospitals, but for the general public wearing personal protective equipment during epidemics or pandemics, respirators provide the greatest source control, followed by surgical masks, with cloth face masks recommended for use by the public only when there are shortages of both respirators and surgical masks.
The following outline is provided as an overview of and topical guide to concepts related to infectious diseases in humans.