Related Research Articles

The aorta is the main and largest artery in the human body, originating from the left ventricle of the heart, branching upwards immediately after, and extending down to the abdomen, where it splits at the aortic bifurcation into two smaller arteries. The aorta distributes oxygenated blood to all parts of the body through the systemic circulation.
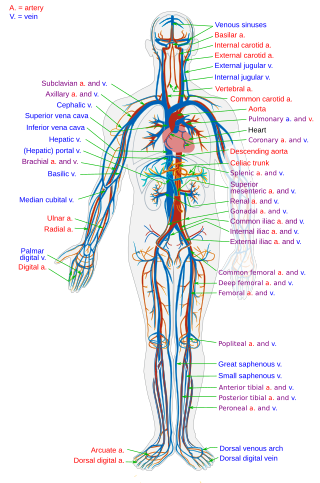
The circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, that consists of the heart and blood vessels. The circulatory system has two divisions, a systemic circulation or circuit, and a pulmonary circulation or circuit. Some sources use the terms cardiovascular system and vascular system interchangeably with circulatory system.

Coronary artery bypass surgery, also known as coronary artery bypass graft, is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pain caused by CAD, slow the progression of CAD, and increase life expectancy. It aims to bypass narrowings in heart arteries by using arteries or veins harvested from other parts of the body, thus restoring adequate blood supply to the previously ischemic heart.

The aortic valve is a valve in the heart of humans and most other animals, located between the left ventricle and the aorta. It is one of the four valves of the heart and one of the two semilunar valves, the other being the pulmonary valve. The aortic valve normally has three cusps or leaflets, although in 1–2% of the population it is found to congenitally have two leaflets. The aortic valve is the last structure in the heart the blood travels through before stopping the flow through the systemic circulation.

Heart murmurs are unique heart sounds produced when blood flows across a heart valve or blood vessel. This occurs when turbulent blood flow creates a sound loud enough to hear with a stethoscope. The sound differs from normal heart sounds by their characteristics. For example, heart murmurs may have a distinct pitch, duration and timing. The major way health care providers examine the heart on physical exam is heart auscultation; another clinical technique is palpation, which can detect by touch when such turbulence causes the vibrations called cardiac thrill. A murmur is a sign found during the cardiac exam. Murmurs are of various types and are important in the detection of cardiac and valvular pathologies.

Cardiopulmonary bypass (CPB) or heart-lung machine also called the pump or CPB pump is a machine that temporarily takes over the function of the heart and lungs during open-heart surgery by maintaining the circulation of blood and oxygen throughout the body. As such it is an extracorporeal device.

A ventricle is one of two large chambers located toward the bottom of the heart that collect and expel blood towards the peripheral beds within the body and lungs. The blood pumped by a ventricle is supplied by an atrium, an adjacent chamber in the upper heart that is smaller than a ventricle. Interventricular means between the ventricles, while intraventricular means within one ventricle.

dextro-Transposition of the great arteries is a potentially life-threatening birth defect in the large arteries of the heart. The primary arteries are transposed.

Aortic regurgitation (AR), also known as aortic insufficiency (AI), is the leaking of the aortic valve of the heart that causes blood to flow in the reverse direction during ventricular diastole, from the aorta into the left ventricle. As a consequence, the cardiac muscle is forced to work harder than normal.

A transesophageal echocardiogram is an alternative way to perform an echocardiogram. A specialized probe containing an ultrasound transducer at its tip is passed into the patient's esophagus. This allows image and Doppler evaluation which can be recorded. It is commonly used during cardiac surgery and is an excellent modality for assessing the aorta, although there are some limitations.

Coarctation of the aorta (CoA) is a congenital condition whereby the aorta is narrow, usually in the area where the ductus arteriosus inserts. The word coarctation means "pressing or drawing together; narrowing". Coarctations are most common in the aortic arch. The arch may be small in babies with coarctations. Other heart defects may also occur when coarctation is present, typically occurring on the left side of the heart. When a patient has a coarctation, the left ventricle has to work harder. Since the aorta is narrowed, the left ventricle must generate a much higher pressure than normal in order to force enough blood through the aorta to deliver blood to the lower part of the body. If the narrowing is severe enough, the left ventricle may not be strong enough to push blood through the coarctation, thus resulting in a lack of blood to the lower half of the body. Physiologically its complete form is manifested as interrupted aortic arch.
Aortic valve replacement is a cardiac surgery procedure whereby a failing aortic valve is replaced with an artificial heart valve. The aortic valve may need to be replaced because of aortic regurgitation, or if the valve is narrowed by stenosis.

The Norwood procedure is the first of three surgeries intended to create a new functional systemic circuit in patients with hypoplastic left heart syndrome (HLHS) and other complex heart defects with single ventricle physiology. The first successful Norwood procedure involving the use of a cardiopulmonary bypass was reported by Dr. William Imon Norwood, Jr. and colleagues in 1981.

Arterial switch operation (ASO) or arterial switch, is an open heart surgical procedure used to correct dextro-transposition of the great arteries (d-TGA).
Cardioplegia is a solution given to the heart during cardiac surgery, to minimize the damage caused by myocardial ischemia while the heart is paused.
Deep hypothermic circulatory arrest (DHCA) is a surgical technique in which the temperature of the body falls significantly and blood circulation is stopped for up to one hour. It is used when blood circulation to the brain must be stopped because of delicate surgery within the brain, or because of surgery on large blood vessels that lead to or from the brain. DHCA is used to provide a better visual field during surgery due to the cessation of blood flow. DHCA is a form of carefully managed clinical death in which heartbeat and all brain activity cease.
Lars Georg Svensson is a cardiac surgeon and the chairman of the heart and vascular institute at Cleveland Clinic. He is the Director of the Aorta Center, Director of the Marfan Syndrome and Connective Tissue Disorder Clinic, and is a professor of surgery at Cleveland Clinic Lerner College of Medicine and Case Western Reserve University. He is also the Director of Quality Outcomes and Process Improvement for the Department of Thoracic and Cardiovascular Surgery and Affiliate Cardiac Surgery Program at Cleveland Clinic.

Open aortic surgery (OAS), also known as open aortic repair (OAR), describes a technique whereby an abdominal, thoracic or retroperitoneal surgical incision is used to visualize and control the aorta for purposes of treatment, usually by the replacement of the affected segment with a prosthetic graft. OAS is used to treat aneurysms of the abdominal and thoracic aorta, aortic dissection, acute aortic syndrome, and aortic ruptures. Aortobifemoral bypass is also used to treat atherosclerotic disease of the abdominal aorta below the level of the renal arteries. In 2003, OAS was surpassed by endovascular aneurysm repair (EVAR) as the most common technique for repairing abdominal aortic aneurysms in the United States.

Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a minimally invasive procedure performed during resuscitation of critically injured trauma patients. Originally developed as a less invasive alternative to emergency thoracotomy with aortic cross clamping, REBOA is performed to gain rapid control of non-compressible truncal or junctional hemorrhage. REBOA is performed first by achieving access to the common femoral artery (CFA) and advancing a catheter within the aorta. Upon successful catheter placement, an occluding balloon may be inflated either within the descending thoracic aorta or infrarenal abdominal aorta. REBOA stanches downstream hemorrhage and improves cardiac index, cerebral perfusion, and coronary perfusion. Although REBOA does not eliminate the need for definitive hemorrhage control, it may serve as a temporizing measure during initial resuscitation. Despite the benefits of REBOA, there are significant local and systemic ischemic risks. Establishing standardized REBOA procedural indications and mitigating the risk of ischemic injury are topics of ongoing investigation. Although this technique has been successfully deployed in adult patients, it has not yet been studied in children.
The Yasui procedure is a pediatric heart operation used to bypass the left ventricular outflow tract (LVOT) that combines the aortic repair of the Norwood procedure and a shunt similar to that used in the Rastelli procedure in a single operation. It is used to repair defects that result in the physiology of hypoplastic left heart syndrome even though both ventricles are functioning normally. These defects are common in DiGeorge syndrome and include interrupted aortic arch and LVOT obstruction (IAA/LVOTO); aortic atresia-severe stenosis with ventricular septal defect (AA/VSD); and aortic atresia with interrupted aortic arch and aortopulmonary window. This procedure allows the surgeon to keep the left ventricle connected to the systemic circulation while using the pulmonary valve as its outflow valve, by connecting them through the ventricular septal defect. The Yasui procedure includes a modified Damus–Kaye–Stansel procedure to connect the aortic and pulmonary roots, allowing the coronary arteries to remain perfused. It was first described in 1987.