Childbirth, also known as labour and delivery, is the ending of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or Caesarean section. In 2019, there were about 140.11 million births globally. In the developed world most deliveries occur in hospitals, while in the developing world most were at home births.

Maternal death or maternal mortality is defined in slightly different ways by several different health organizations. The World Health Organization (WHO) defines maternal death as the death of a pregnant woman due to complications related to pregnancy, underlying conditions worsened by the pregnancy or management of these conditions. This can occur either while she is pregnant or within six weeks of resolution of the pregnancy. The CDC definition of pregnancy-related deaths extends the period of consideration to include one year from the resolution of the pregnancy. Pregnancy associated death, as defined by the American College of Obstetricians and Gynecologists (ACOG), are all deaths occurring within one year of a pregnancy resolution. Identification of pregnancy associated deaths is important for deciding whether or not the pregnancy was a direct or indirect contributing cause of the death.

Preterm birth, also known as premature birth, is the birth of a baby at fewer than 37 weeks gestational age, as opposed to full-term delivery at approximately 40 weeks. Extreme preterm is less than 28 weeks, very early preterm birth is between 28 and 32 weeks, early preterm birth occurs between 32 and 36 weeks, late preterm birth is between 34 and 36 weeks' gestation. These babies are also known as premature babies or colloquially preemies or premmies. Symptoms of preterm labor include uterine contractions which occur more often than every ten minutes and/or the leaking of fluid from the vagina before 37 weeks. Premature infants are at greater risk for cerebral palsy, delays in development, hearing problems and problems with their vision. The earlier a baby is born, the greater these risks will be.

A neonatal intensive care unit (NICU), also known as an intensive care nursery (ICN), is an intensive care unit (ICU) specializing in the care of ill or premature newborn infants. Neonatal refers to the first 28 days of life. Neonatal care, as known as specialized nurseries or intensive care, has been around since the 1960s.
Fetal viability is the ability of a human fetus to survive outside the uterus. Medical viability is generally considered to be between 23 and 24 weeks gestational age. Viability depends upon factors such as birth weight, gestational age, and the availability of advanced medical care. In low-income countries, half of newborns born at or below 32 weeks gestational age died due a lack of medical access; in high-income countries, the vast majority of newborns born above 24 weeks gestational age survive.
In obstetrics, gestational age is a measure of the age of a pregnancy which is taken from the beginning of the woman's last menstrual period (LMP), or the corresponding age of the gestation as estimated by a more accurate method if available. Such methods include adding 14 days to a known duration since fertilization, or by obstetric ultrasonography. The popularity of using this definition of gestational age is that menstrual periods are essentially always noticed, while there is usually a lack of a convenient way to discern when fertilization occurred. "Gestational age" in other contexts may mean embryonic age.

Pregnancy is the time during which one or more offspring develops (gestates) inside a woman's womb. A multiple pregnancy involves more than one offspring, such as with twins. Pregnancy usually occurs by sexual intercourse, but can also occur through assisted reproductive technology procedures. A pregnancy may end in a live birth, a spontaneous miscarriage, an induced abortion, or a stillbirth. Childbirth typically occurs around 40 weeks from the start of the last menstrual period (LMP), a span known as the gestational age. This is just over nine months. Counting by fertilization age, the length is about 38 weeks. Pregnancy is "the presence of an implanted human embryo or fetus in the uterus"; implantation occurs on average 8–9 days after fertilization. An embryo is the term for the developing offspring during the first seven weeks following implantation, after which the term fetus is used until birth. Signs and symptoms of early pregnancy may include missed periods, tender breasts, morning sickness, hunger, and frequent urination. Pregnancy may be confirmed with a pregnancy test. Methods of birth control—or, more accurately, contraception—are used to avoid pregnancy.

Low birth weight (LBW) is defined by the World Health Organization as a birth weight of an infant of 2,499 g or less, regardless of gestational age. Infants born with LBW have added health risks which require close management, often in a neonatal intensive care unit (NICU). They are also at increased risk for long-term health conditions which require follow-up over time.

Birth weight is the body weight of a baby at its birth. The average birth weight in babies of European descent is 3.5 kilograms (7.7 lb), with the normative range between 2.5 and 4.5 kilograms. On average, babies of South Asian and Chinese descent weigh about 3.26 kilograms (7.2 lb). As far as low birth weight prevalence rates changing over time, there has been a slight decrease from 7.9% (1970) to 6.8% (1980), then a slight increase to 8.3% (2006), to the current levels of 8.2% (2016). The prevalence of low birth weights has trended slightly upward from 2012 to the present.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labor. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.

Complications of pregnancy are health problems that are related to pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. Severe complications of pregnancy, childbirth, and the puerperium are present in 1.6% of mothers in the US, and in 1.5% of mothers in Canada. In the immediate postpartum period (puerperium), 87% to 94% of women report at least one health problem. Long-term health problems are reported by 31% of women.
Antenatal steroids, also known as antenatal corticosteroids, are medications administered to pregnant women expecting a preterm birth. When administered, these steroids accelerate the maturation of the fetus' lungs, which reduces the likelihood of infant respiratory distress syndrome and infant mortality. The effectiveness of this corticosteroid treatment on humans was first demonstrated in 1972 by Sir Graham Liggins and Ross Howie, during a randomized control trial using betamethasone.
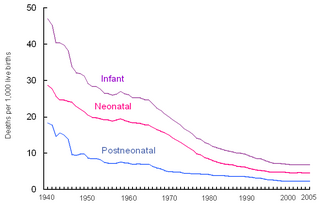
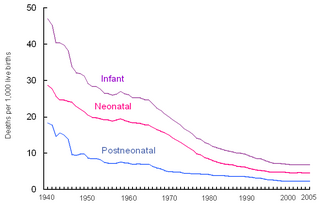
Perinatal mortality (PNM) refers to the death of a fetus or neonate and is the basis to calculate the perinatal mortality rate. Variations in the precise definition of the perinatal mortality exist, specifically concerning the issue of inclusion or exclusion of early fetal and late neonatal fatalities. The World Health Organization defines perinatal mortality as the "number of stillbirths and deaths in the first week of life per 1,000 total births, the perinatal period commences at 22 completed weeks of gestation, and ends seven completed days after birth", but other definitions have been used.
Maternal health is the health of women during pregnancy, childbirth, and the postpartum period. In most cases, it encompasses the health care dimensions of family planning, preconception, prenatal, and postnatal care in order to ensure a positive and fulfilling experience. In other cases, maternal health can reduce maternal morbidity and mortality. Maternal health revolves around the health and wellness of women, particularly when they are pregnant, at the time they give birth, and during child-raising. WHO has indicated that even though motherhood has been considered as a fulfilling natural experience that is emotional to the mother, a high percentage of women develop health problems and sometimes even die. Because of this, there is a need to invest in the health of women. The investment can be achieved in different ways, among the main ones being subsidizing the healthcare cost, education on maternal health, encouraging effective family planning, and ensuring progressive check up on the health of women with children. Maternal mortality particularly affects women of color and women living in low and lower-middle income countries.

Maternal–fetal medicine (MFM), also known as perinatology, is a branch of medicine that focuses on managing health concerns of the mother and fetus prior to, during, and shortly after pregnancy.
The following outline is provided as an overview of and topical guide to obstetrics:

A high-risk pregnancy is one where the mother or the fetus has an increased risk of adverse outcomes compared to uncomplicated pregnancies. No concrete guidelines currently exist for distinguishing “high-risk” pregnancies from “low-risk” pregnancies, however there are certain studied conditions that have been shown to put the mother or fetus at a higher risk of poor outcomes. These conditions can be classified into three main categories: health problems in the mother that occur before she becomes pregnant, health problems in the mother that occur during pregnancy, and certain health conditions with the fetus.
A pre-existing disease in pregnancy is a disease that is not directly caused by the pregnancy, in contrast to various complications of pregnancy, but which may become worse or be a potential risk to the pregnancy. A major component of this risk can result from necessary use of drugs in pregnancy to manage the disease.
Late preterm infants are infants born at a gestational age between 34+0⁄7 weeks and 36+6⁄7 weeks. They have higher morbidity and mortality rates than term infants due to their relative physiologic and metabolic immaturity, even though they are often the size and weight of some term infants. "Late preterm" has replaced "near term" to describe this group of infants, since near term incorrectly implies that these infants are "almost term" and only require routine neonatal care.

The effect of COVID-19 infection on pregnancy is not completely known because of the lack of reliable data. If there is increased risk to pregnant women and fetuses, so far it has not been readily detectable.