Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

Spina bifida is a birth defect in which there is incomplete closing of the spine and the membranes around the spinal cord during early development in pregnancy. There are three main types: spina bifida occulta, meningocele and myelomeningocele. Meningocele and myelomeningocele may be grouped as spina bifida cystica. The most common location is the lower back, but in rare cases it may be in the middle back or neck.

Colpocephaly is a cephalic disorder involving the disproportionate enlargement of the occipital horns of the lateral ventricles and is usually diagnosed early after birth due to seizures. It is a nonspecific finding and is associated with multiple neurological syndromes, including agenesis of the corpus callosum, Chiari malformation, lissencephaly, and microcephaly. Although the exact cause of colpocephaly is not known yet, it is commonly believed to occur as a result of neuronal migration disorders during early brain development, intrauterine disturbances, perinatal injuries, and other central nervous system disorders. Individuals with colpocephaly have various degrees of motor disabilities, visual defects, spasticity, and moderate to severe intellectual disability. No specific treatment for colpocephaly exists, but patients may undergo certain treatments to improve their motor function or intellectual disability.
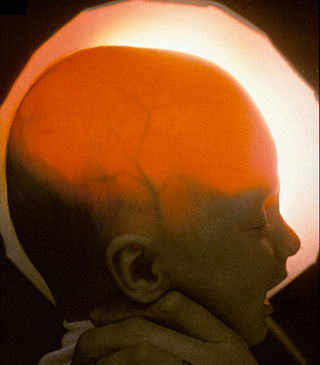
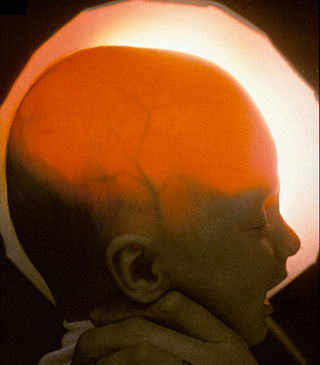
Hydranencephaly is a condition in which the brain's cerebral hemispheres are absent to a great degree and the remaining cranial cavity is filled with cerebrospinal fluid. "Cephalic" is the scientific term for "head" or "head end of body".
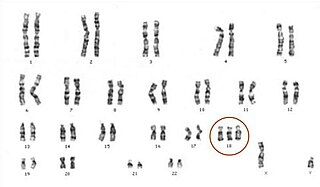
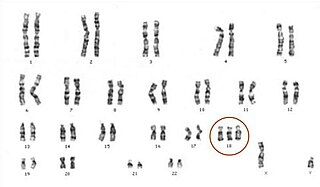
Edwards syndrome, also known as trisomy 18, is a genetic disorder caused by the presence of a third copy of all or part of chromosome 18. Many parts of the body are affected. Babies are often born small and have heart defects. Other features include a small head, small jaw, clenched fists with overlapping fingers, and severe intellectual disability.
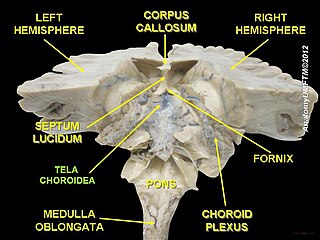
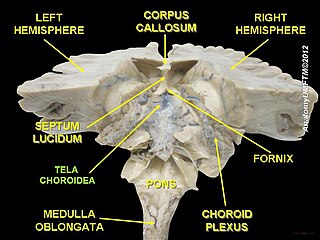
The choroid plexus, or plica choroidea, is a plexus of cells that arises from the tela choroidea in each of the ventricles of the brain. Regions of the choroid plexus produce and secrete most of the cerebrospinal fluid (CSF) of the central nervous system. The choroid plexus consists of modified ependymal cells surrounding a core of capillaries and loose connective tissue. Multiple cilia on the ependymal cells move to circulate the cerebrospinal fluid.
Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of prenatal care that focus on detecting problems with the pregnancy as early as possible. These may be anatomic and physiologic problems with the health of the zygote, embryo, or fetus, either before gestation even starts or as early in gestation as practicable. Screening can detect problems such as neural tube defects, chromosome abnormalities, and gene mutations that would lead to genetic disorders and birth defects, such as spina bifida, cleft palate, Down syndrome, Tay–Sachs disease, sickle cell anemia, thalassemia, cystic fibrosis, muscular dystrophy, and fragile X syndrome. Some tests are designed to discover problems which primarily affect the health of the mother, such as PAPP-A to detect pre-eclampsia or glucose tolerance tests to diagnose gestational diabetes. Screening can also detect anatomical defects such as hydrocephalus, anencephaly, heart defects, and amniotic band syndrome.

Polyhydramnios is a medical condition describing an excess of amniotic fluid in the amniotic sac. It is seen in about 1% of pregnancies. It is typically diagnosed when the amniotic fluid index (AFI) is greater than 24 cm. There are two clinical varieties of polyhydramnios: chronic polyhydramnios where excess amniotic fluid accumulates gradually, and acute polyhydramnios where excess amniotic fluid collects rapidly.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labor. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.

Dandy–Walker malformation (DWM), also known as Dandy–Walker syndrome (DWS), is a rare congenital brain malformation in which the part joining the two hemispheres of the cerebellum does not fully form, and the fourth ventricle and space behind the cerebellum are enlarged with cerebrospinal fluid. Most of those affected develop hydrocephalus within the first year of life, which can present as increasing head size, vomiting, excessive sleepiness, irritability, downward deviation of the eyes and seizures. Other, less common symptoms are generally associated with comorbid genetic conditions and can include congenital heart defects, eye abnormalities, intellectual disability, congenital tumours, other brain defects such as agenesis of the corpus callosum, skeletal abnormalities, an occipital encephalocele or underdeveloped genitalia or kidneys. It is sometimes discovered in adolescents or adults due to mental health problems.

Ventriculomegaly is a brain condition that mainly occurs in the fetus when the lateral ventricles become dilated. The most common definition uses a width of the atrium of the lateral ventricle of greater than 10 mm. This occurs in around 1% of pregnancies. When this measurement is between 10 and 15 mm, the ventriculomegaly may be described as mild to moderate. When the measurement is greater than 15mm, the ventriculomegaly may be classified as more severe.

A nuchal scan or nuchal translucency (NT) scan/procedure is a sonographic prenatal screening scan (ultrasound) to detect chromosomal abnormalities in a fetus, though altered extracellular matrix composition and limited lymphatic drainage can also be detected.
Placental insufficiency or utero-placental insufficiency is the failure of the placenta to deliver sufficient nutrients to the fetus during pregnancy, and is often a result of insufficient blood flow to the placenta. The term is also sometimes used to designate late decelerations of fetal heart rate as measured by cardiotocography or an NST, even if there is no other evidence of reduced blood flow to the placenta, normal uterine blood flow rate being 600mL/min.
Confined placental mosaicism (CPM) represents a discrepancy between the chromosomal makeup of the cells in the placenta and the cells in the fetus. CPM was first described by Kalousek and Dill in 1983. CPM is diagnosed when some trisomic cells are detected on chorionic villus sampling and only normal cells are found on a subsequent prenatal test, such as amniocentesis or fetal blood sampling. In theory, CPM is when the trisomic cells are found only in the placenta. CPM is detected in approximately 1-2% of ongoing pregnancies that are studied by chorionic villus sampling (CVS) at 10 to 12 weeks of pregnancy. Chorionic villus sampling is a prenatal procedure which involves a placental biopsy. Most commonly when CPM is found it represents a trisomic cell line in the placenta and a normal diploid chromosome complement in the baby. However, the fetus is involved in about 10% of cases.
Amnioinfusion is a method in which isotonic fluid is instilled into the uterine cavity.
Theca lutein cyst is a type of bilateral functional ovarian cyst filled with clear, straw-colored fluid. These cysts result from exaggerated physiological stimulation due to elevated levels of beta-human chorionic gonadotropin (beta-hCG) or hypersensitivity to beta-hCG. On ultrasound and MRI, theca lutein cysts appear in multiples on ovaries that are enlarged.

A high-risk pregnancy is one where the mother or the fetus has an increased risk of adverse outcomes compared to uncomplicated pregnancies. No concrete guidelines currently exist for distinguishing “high-risk” pregnancies from “low-risk” pregnancies, however there are certain studied conditions that have been shown to put the mother or fetus at a higher risk of poor outcomes. These conditions can be classified into three main categories: health problems in the mother that occur before she becomes pregnant, health problems in the mother that occur during pregnancy, and certain health conditions with the fetus.
Cell-free fetal DNA (cffDNA) is fetal DNA that circulates freely in the maternal blood. Maternal blood is sampled by venipuncture. Analysis of cffDNA is a method of non-invasive prenatal diagnosis frequently ordered for pregnant women of advanced maternal age. Two hours after delivery, cffDNA is no longer detectable in maternal blood.
The anomaly scan, also sometimes called the anatomy scan, 20-week ultrasound, or level 2 ultrasound, evaluates anatomic structures of the fetus, placenta, and maternal pelvic organs. This scan is an important and common component of routine prenatal care. The function of the ultrasound is to measure the fetus so that growth abnormalities can be recognized quickly later in pregnancy, to assess for congenital malformations and multiple pregnancies, and to plan method of delivery.
Beryl Rice Benacerraf was an American radiologist and professor of obstetrics, gynecology and reproductive biology and radiology at Harvard Medical School. She was a pioneer in the use of prenatal ultrasound to diagnose fetal abnormalities, including Down syndrome. In 2021, she was recognized as a "Giant in Obstetrics and Gynecology" by the American Journal of Obstetrics & Gynecology.