An action potential occurs when the membrane potential of a specific cell rapidly rises and falls. This depolarization then causes adjacent locations to similarly depolarize. Action potentials occur in several types of animal cells, called excitable cells, which include neurons, muscle cells, and in some plant cells. Certain endocrine cells such as pancreatic beta cells, and certain cells of the anterior pituitary gland are also excitable cells.
An evoked potential or evoked response is an electrical potential in a specific pattern recorded from a specific part of the nervous system, especially the brain, of a human or other animals following presentation of a stimulus such as a light flash or a pure tone. Different types of potentials result from stimuli of different modalities and types. Evoked potential is distinct from spontaneous potentials as detected by electroencephalography (EEG), electromyography (EMG), or other electrophysiologic recording method. Such potentials are useful for electrodiagnosis and monitoring that include detections of disease and drug-related sensory dysfunction and intraoperative monitoring of sensory pathway integrity.

An electrical injury, or electrical shock is damage sustained to the skin or internal organs on direct contact with an electric current.

In physiology, a stimulus is a detectable change in the physical or chemical structure of an organism's internal or external environment. The ability of an organism or organ to detect external stimuli, so that an appropriate reaction can be made, is called sensitivity (excitability). Sensory receptors can receive information from outside the body, as in touch receptors found in the skin or light receptors in the eye, as well as from inside the body, as in chemoreceptors and mechanoreceptors. When a stimulus is detected by a sensory receptor, it can elicit a reflex via stimulus transduction. An internal stimulus is often the first component of a homeostatic control system. External stimuli are capable of producing systemic responses throughout the body, as in the fight-or-flight response. In order for a stimulus to be detected with high probability, its level of strength must exceed the absolute threshold; if a signal does reach threshold, the information is transmitted to the central nervous system (CNS), where it is integrated and a decision on how to react is made. Although stimuli commonly cause the body to respond, it is the CNS that finally determines whether a signal causes a reaction or not.

Functional electrical stimulation (FES) is a technique that uses low-energy electrical pulses to artificially generate body movements in individuals who have been paralyzed due to injury to the central nervous system. More specifically, FES can be used to generate muscle contraction in otherwise paralyzed limbs to produce functions such as grasping, walking, bladder voiding and standing. This technology was originally used to develop neuroprostheses that were implemented to permanently substitute impaired functions in individuals with spinal cord injury (SCI), head injury, stroke and other neurological disorders. In other words, a person would use the device each time he or she wanted to generate a desired function. FES is sometimes also referred to as neuromuscular electrical stimulation (NMES).
Axonotmesis is an injury to the peripheral nerve of one of the extremities of the body. The axons and their myelin sheath are damaged in this kind of injury, but the endoneurium, perineurium and epineurium remain intact. Motor and sensory functions distal to the point of injury are completely lost over time leading to Wallerian degeneration due to ischemia, or loss of blood supply. Axonotmesis is usually the result of a more severe crush or contusion than neurapraxia.
The H-reflex is a reflectory reaction of muscles after electrical stimulation of sensory fibers in their innervating nerves. The H-reflex test is performed using an electric stimulator, which gives usually a square-wave current of short duration and small amplitude, and an EMG set, to record the muscle response. That response is usually a clear wave, called H-wave, 28-35 ms after the stimulus, not to be confused with an F-wave. An M-wave, an early response, occurs 3-6 ms after the onset of stimulation. The H and F-waves are later responses. As the stimulus increases, the amplitude of the F-wave increases only slightly, and the H-wave decreases, and at supramaximal stimulus, the H-wave will disappear. The M-wave does the opposite of the H-wave. As the stimulus increases the M-wave increases. There is a point of minimal stimulus where the M-wave is absent and the H-wave is maximal.
Pulpitis is inflammation of dental pulp tissue. The pulp contains the blood vessels, the nerves, and connective tissue inside a tooth and provides the tooth's blood and nutrients. Pulpitis is mainly caused by bacterial infection which itself is a secondary development of caries. It manifests itself in the form of a toothache.
Neural engineering is a discipline within biomedical engineering that uses engineering techniques to understand, repair, replace, or enhance neural systems. Neural engineers are uniquely qualified to solve design problems at the interface of living neural tissue and non-living constructs.

Electrosurgery is the application of a high-frequency alternating polarity, electrical current to biological tissue as a means to cut, coagulate, desiccate, or fulgurate tissue. Its benefits include the ability to make precise cuts with limited blood loss. Electrosurgical devices are frequently used during surgical operations helping to prevent blood loss in hospital operating rooms or in outpatient procedures.

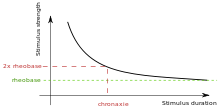
Rheobase is a measure of membrane potential excitability. In neuroscience, rheobase is the minimal current amplitude of infinite duration that results in the depolarization threshold of the cell membranes being reached, such as an action potential or the contraction of a muscle. In Greek, the root rhe translates to "current or flow", and basi means "bottom or foundation": thus the rheobase is the minimum current that will produce an action potential or muscle contraction.
In physiology, the all-or-none law is the principle that if a single nerve fibre is stimulated, it will always give a maximal response and produce an electrical impulse of a single amplitude. If the intensity or duration of the stimulus is increased, the height of the impulse will remain the same. The nerve fibre either gives a maximal response or none at all.

Group C nerve fibers are one of three classes of nerve fiber in the central nervous system (CNS) and peripheral nervous system (PNS). The C group fibers are unmyelinated and have a small diameter and low conduction velocity, whereas Groups A and B are myelinated. Group C fibers include postganglionic fibers in the autonomic nervous system (ANS), and nerve fibers at the dorsal roots. These fibers carry sensory information.

Denervation is any loss of nerve supply regardless of the cause. If the nerves lost to denervation are part of the neuronal communication to a specific function in the body then altered or a loss of physiological functioning can occur. Denervation can be caused by injury or be a symptom of a disorder like ALS, post-polio syndrome, or POTS. Additionally, it can be a useful surgical technique to alleviate major negative symptoms, such as in renal denervation. Denervation can have many harmful side effects such as increased risk of infection and tissue dysfunction.
Clinical electrophysiology is the application of electrophysiology principles to medicine. The two main branches of this discipline are electrotherapy and electrophysiologic testing Clinical electrophysiology can be utilized in the study and treatment of various physiological conditions, and most notably in clinical cardiac electrophysiology.
Repetitive nerve stimulation is a variant of the nerve conduction study where electrical stimulation is delivered to a motor nerve repeatedly several times per second. By observing the change in the muscle electrical response (CMAP) after several stimulations, a physician can assess for the presence of a neuromuscular junction disease, and differentiate between presynaptic and postsynaptic conditions. The test was first described by German neurologist Friedrich Jolly in 1895, and is also known as Jolly's test.
Electroanalgesia is a form of analgesia, or pain relief, that uses electricity to ease pain. Electrical devices can be internal or external, at the site of pain (local) or delocalized throughout the whole body. It works by interfering with the electric currents of pain signals, inhibiting them from reaching the brain and inducing a response; different from traditional analgesics, such as opiates which mimic natural endorphins and NSAIDs that help relieve inflammation and stop pain at the source. Electroanalgesia has a lower addictive potential and poses less health threats to the general public, but can cause serious health problems, even death, in people with other electrical devices such as pacemakers or internal hearing aids, or with heart problems.
A depolarizing prepulse (DPP) is an electrical stimulus that causes the potential difference measured across a neuronal membrane to become more positive or less negative, and precedes another electrical stimulus. DPPs may be of either the voltage or current stimulus variety and have been used to inhibit neural activity, selectively excite neurons, and increase the pain threshold associated with electrocutaneous stimulation.
Neurostimulation is the purposeful modulation of the nervous system's activity using invasive or non-invasive means. Neurostimulation usually refers to the electromagnetic approaches to neuromodulation.

The Shannon criteria constitute an empirical rule in neural engineering that is used for evaluation of possibility of damage from electrical stimulation to nervous tissue.