A subluxation is an incomplete or partial dislocation of a joint or organ. According to the World Health Organization, a subluxation is a "significant structural displacement" and is therefore visible on static imaging studies, such as X-rays. Unlike real subluxations, the pseudoscientific concept of a chiropractic "vertebral subluxation" may or may not be visible on x-rays.

Ehlers–Danlos syndromes (EDS) are a group of 13 genetic connective-tissue disorders. Symptoms often include loose joints, joint pain, stretchy velvety skin, and abnormal scar formation. These may be noticed at birth or in early childhood. Complications may include aortic dissection, joint dislocations, scoliosis, chronic pain, or early osteoarthritis. The current classification was last updated in 2017, when a number of rarer forms of EDS were added.

In neurology, the Chiari malformation is a structural defect in the cerebellum, characterized by a downward displacement of one or both cerebellar tonsils through the foramen magnum.

Cervical spine disorders are illnesses that affect the cervical spine, which is made up of the upper first seven vertebrae, encasing and shielding the spinal cord. This fragment of the spine starts from the region above the shoulder blades and ends by supporting and connecting the skull.

Klippel–Feil syndrome (KFS), also known as cervical vertebral fusion syndrome, is a rare congenital condition characterized by the abnormal fusion of any two of the seven bones in the neck. It can result in a limited ability to move the neck and shortness of the neck, resulting in the appearance of a low hairline. Most people only have one or two of those symptoms so it may not be noticeable without medical imaging.

Ligamentous laxity, or ligament laxity, is a cause of chronic body pain characterized by loose ligaments. When this condition affects joints in the entire body, it is called generalized joint hypermobility, which occurs in about ten percent of the population, and may be genetic. Loose ligaments can appear in a variety of ways and levels of severity. It also does not always affect the entire body. One could have loose ligaments of the feet, but not of the arms.
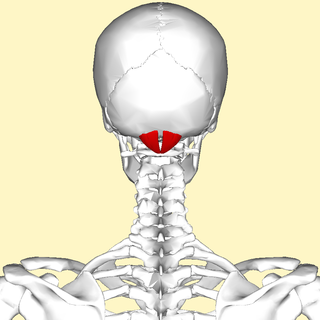
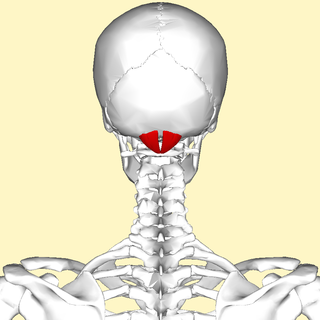
The rectus capitis posterior minor is a muscle in the upper back part of the neck. It is one of the suboccipital muscles. Its inferior attachment is at the posterior arch of atlas; its superior attachment is onto the occipital bone at and below the inferior nuchal line. The muscle is innervated by the suboccipital nerve. The muscle acts as a weak extensor of the head.

Hypermobility, also known as double-jointedness, describes joints that stretch farther than normal. For example, some hypermobile people can bend their thumbs backwards to their wrists and bend their knee joints backwards, put their leg behind the head or perform other contortionist "tricks". It can affect one or more joints throughout the body.

Hypermobility spectrum disorder (HSD), related to earlier diagnoses such as hypermobility syndrome (HMS), and joint hypermobility syndrome (JHS) is a heritable connective tissue disorder that affects joints and ligaments. Different forms and sub-types have been distinguished, but it does not include asymptomatic joint hypermobility, sometimes known as double-jointedness.

In anatomy, the transverse ligament of the atlas is a broad, tough ligament which arches across the ring of the atlas posterior to the dens to keep the dens in contact with the atlas. It forms the transverse component of the cruciform ligament of atlas.

The occipital condyles are undersurface protuberances of the occipital bone in vertebrates, which function in articulation with the superior facets of the atlas vertebra.
Atlanto-occipital dislocation, orthopedic decapitation, or internal decapitation describes ligamentous separation of the spinal column from the skull base. It is possible for a human to survive such an injury; however, 70% of cases result in immediate death. It should not be confused with atlanto-axial dislocation, which describes ligamentous separation between the first and second cervical vertebra.

The cruciate ligament of the atlas is a cross-shaped ligament in the neck forming part of the atlanto-axial joint. It consists of the transverse ligament of atlas, a superior longitudinal band, and an inferior longitudinal band.

Tenascin X (TN-X), also known as flexillin or hexabrachion-like protein, is a 450kDa glycoprotein, a member of the tenascin family, that is expressed in connective tissues. In humans it is encoded by the TNXB gene.

A cerebrospinal fluid leak is a medical condition where the cerebrospinal fluid (CSF) that surrounds the brain and spinal cord leaks out of one or more holes or tears in the dura mater. A CSF leak is classed as either spontaneous (primary), having no known cause, or nonspontaneous (secondary) where it is attributed to an underlying condition. Causes of a primary CSF leak are those of trauma including from an accident or intentional injury, or arising from a medical intervention known as iatrogenic. A basilar skull fracture as a cause can give the sign of CSF leakage from the ear, nose or mouth. A lumbar puncture can give the symptom of a post-dural-puncture headache.
The Chiari Institute is a medical institution that focuses on the treatment of Arnold–Chiari malformation and syringomyelia. It was established in 2001 by the North Shore-LIJ Health System, and is located in Great Neck, New York. The institute was founded by Thomas H. Milhorat, MD shortly after he was appointed the Chairman of Neurosurgery at the North Shore-Long Island Jewish Health System, and Paolo Bolognese, MD. It is now led by Raj Narayan, MD. Paolo Bolognese left TCI on September, 1st, 2014

Cervicocranial syndrome or is a combination of symptoms that are caused by an abnormality in the cervical vertebrae leading to improper function of cervical spinal nerves. Cervicocranial syndrome is either congenital or acquired. Cervicocranial syndrome may be caused by Chiari disease, Klippel-Feil malformation, osteoarthritis, and physical trauma. Treatment options include neck braces, pain medication and surgery. The quality of life for individuals suffering from Cervicocranial syndrome can improve through surgery.

Rheumatoid disease of the spine is a morbid consequence of untreated longstanding severe cervical spinal rheumatoid arthritis (RA)–an inflammatory autoimmune disease that attacks the ligaments, joints, and bones of the neck. Although the anterior subluxation of the atlantoaxial joint is the most common manifestation of the disorder, subluxation can also occur with posterior or vertical movement, and subaxial joints can also be involved.
Neck-tongue syndrome (NTS), which was first recorded in 1980, is a rare disorder characterized by neck pain with or without tingling and numbness of the tongue on the same side as the neck pain. Sharp lateral movement of the head triggers the pain, usually lasting from a few seconds to a few minutes. Headaches may occur with the onset of NTS. The typical age of onset is around adolescence and may occur as early as 8–15 years old. However, clinical onset can occur earlier or later and NTS onset related to trauma can occur at any age, beginning after the incident.
Clair A. Francomano is an American medical geneticist and academic specializing in Ehlers–Danlos syndromes. She is Professor of Medical and Molecular Genetics at Indiana University.