Organ donation is the process when a person authorizes an organ of their own to be removed and transplanted to another person, legally, either by consent while the donor is alive, through a legal authorization for deceased donation made prior to death, or for deceased donations through the authorization by the legal next of kin.

Organ transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transported from a donor site to another location. Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts. Allografts can either be from a living or cadaveric source.

Transplant rejection occurs when transplanted tissue is rejected by the recipient's immune system, which destroys the transplanted tissue. Transplant rejection can be lessened by determining the molecular similitude between donor and recipient and by use of immunosuppressant drugs after transplant.
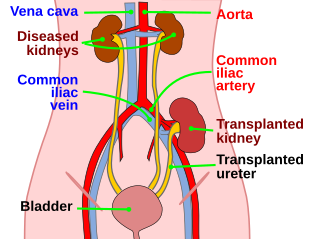
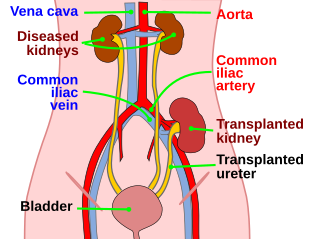
Kidney transplant or renal transplant is the organ transplant of a kidney into a patient with end-stage kidney disease (ESRD). Kidney transplant is typically classified as deceased-donor or living-donor transplantation depending on the source of the donor organ. Living-donor kidney transplants are further characterized as genetically related (living-related) or non-related (living-unrelated) transplants, depending on whether a biological relationship exists between the donor and recipient. The first successful kidney transplant was performed in 1954 by a team including Joseph Murray, the recipient's surgeon, and Hartwell Harrison, surgeon for the donor. Murray was awarded a Nobel Prize in Physiology or Medicine in 1990 for this and other work. In 2018, an estimated 95,479 kidney transplants were performed worldwide, 36% of which came from living donors.

Canadian Blood Services is a non-profit charitable organization that is independent from the Canadian government. The Canadian Blood Services was established as Canada's blood authority in all provinces and territories except for Quebec in 1998. The federal, provincial and territorial governments created the Canadian Blood Services through a memorandum of understanding. Canadian Blood Services is funded mainly through the provincial and territorial governments.

Lung transplantation, or pulmonary transplantation, is a surgical procedure in which one or both lungs are replaced by lungs from a donor. Donor lungs can be retrieved from a living or deceased donor. A living donor can only donate one lung lobe. With some lung diseases, a recipient may only need to receive a single lung. With other lung diseases such as cystic fibrosis, it is imperative that a recipient receive two lungs. While lung transplants carry certain associated risks, they can also extend life expectancy and enhance the quality of life for those with end stage pulmonary disease.

The United Network for Organ Sharing (UNOS) is a non-profit scientific and educational organization that administers the only Organ Procurement and Transplantation Network (OPTN) in the United States, established by the U.S. Congress in 1984 by Gene A. Pierce, founder of United Network for Organ Sharing. Located in Richmond, Virginia, the organization's headquarters are situated near the intersection of Interstate 95 and Interstate 64 in the Virginia BioTechnology Research Park.
Organ procurement is a surgical procedure that removes organs or tissues for reuse, typically for organ transplantation.
Organ trade is the trading of human organs, tissues, or other body products, usually for transplantation. According to the World Health Organization (WHO), organ trade is a commercial transplantation where there is a profit, or transplantations that occur outside of national medical systems. There is a global need or demand for healthy body parts for transplantation, which exceeds the numbers available.
"Harvest" is the 14th episode of the second season of the American television show Numbers. Inspired by a Christian Science Monitor article about organ tourists, people who travel to a different country to give their organs for money, and an algorithm developed in the United States, the episode features Federal Bureau of Investigation (FBI) agents and mathematicians attempting to locate a missing organ tourist before she is killed.

Francis L. Delmonico, MD, FACS is an American surgeon, clinical professor and health expert in the field of transplantation. He serves on numerous committees and is affiliated with various leading organizations and institutions. He is the chief medical officer of the New England Organ Bank (NEOB) and Professor of Surgery, Part-Time at Harvard Medical School in Boston, Massachusetts, where he is emeritus director of renal transplantation. He served as president of The Transplantation Society (TTS) from 2012 to 2014, an international non-profit organization based in Montreal, Canada that works with international transplantation physicians and researchers. He also served as the president of the United Network of Organ Sharing (UNOS) in 2005, which overseas the practice of organ donation and transplantation in the United States. He was appointed and still serves as an advisor to the World Health Organization in matters of organ donation and transplantation. He was appointed by Pope Francis to the Pontifical Academy of Science in 2016. In 2020, he became the recipient of the Medawar Prize of The Transplantation Society.

A heart transplant, or a cardiac transplant, is a surgical transplant procedure performed on patients with end-stage heart failure or severe coronary artery disease when other medical or surgical treatments have failed. As of 2018, the most common procedure is to take a functioning heart, with or without both lungs, from a recently deceased organ donor and implant it into the patient. The patient's own heart is either removed and replaced with the donor heart or, much less commonly, the recipient's diseased heart is left in place to support the donor heart.
ABO-incompatible (ABOi) transplantation is a method of allocation in organ transplantation that permits more efficient use of available organs regardless of ABO blood type, which would otherwise be unavailable due to hyperacute rejection. Primarily in use in infants and young toddlers, research is ongoing to allow for increased use of this capability in adult transplants. Normal ABO-compatibility rules may be observed for all recipients. This means that anyone may receive a transplant of a type-O organ, and consequently, type-O recipients are one of the biggest beneficiaries of ABO-incompatible transplants. While focus has been on infant heart transplants, the principles generally apply to other forms of solid organ transplantation.
Tayfun Sönmez is a Turkish-American professor of economics at Boston College. He is a Fellow of the Econometric Society and the 2008 winner of the Social Choice and Welfare Prize, which honors scholars under the age of 40 for excellent accomplishment in the area of social choice theory and welfare economics. Sönmez has made significant contributions in the areas of microeconomic theory, mechanism/market design, and game theory. His work has been featured by the U.S. National Science Foundation for its practical relevance.

Intestine transplantation is the surgical replacement of the small intestine for chronic and acute cases of intestinal failure. While intestinal failure can oftentimes be treated with alternative therapies such as parenteral nutrition (PN), complications such as PN-associated liver disease and short bowel syndrome may make transplantation the only viable option. One of the rarest type of organ transplantation performed, intestine transplantation is becoming increasingly prevalent as a therapeutic option due to improvements in immunosuppressive regimens, surgical technique, PN, and the clinical management of pre and post-transplant patients.
The National Kidney Registry (NKR) is a national registry in the United States listing kidney donors and recipients in need of a kidney transplant. NKR facilitates over 450 "Kidney Paired Donation" (KPD) or "Paired Exchange" transplants annually.
Kidney paired donation (KPD), or paired exchange, is an approach to living donor kidney transplantation where patients with incompatible donors swap kidneys to receive a compatible kidney. KPD is used in situations where a potential donor is incompatible. Because better donor HLA and age matching are correlated with lower lifetime mortality and longer lasting kidney transplants, many compatible pairs are also participating in swaps to find better matched kidneys. In the United States, the National Kidney Registry organizes the majority of U.S. KPD transplants, including the largest swaps. The first large swap was a 60 participant chain in 2012 that appeared on the front page of the New York Times and the second, even larger swap, included 70 participants and was completed in 2014. Other KPD programs in the U.S. include the UNOS program, which was launched in 2010 and completed its 100th KPD transplant in 2014, and the Alliance for Paired Donation.
Donor-specific antibodies (DSA) are a concept in transplantation medicine and describe the presence of antibodies specific to the Donor's HLA-Molecules. These antibodies can cause antibody-mediated rejection and are therefore considered a contraindication against transplantation in most cases. DSA are a result of B cell and plasma cell activation and bind to HLA and/or non-HLA molecules on the endothelium of the graft. They were first described in 1969 by Patel et al., who found that Transplant recipients who were positively tested for DSA using a complement-dependent cytotoxicity crossmatch assay had a higher risk of transplant rejection. DSA can either be pre-formed or can be formed as a response to the transplantion.
Sommer Elizabeth Gentry is an American mathematician who works as a professor of mathematics at the United States Naval Academy and as a research associate in surgery at the Johns Hopkins School of Medicine. Her research concerns operations research and its applications to the optimization of organ transplants, and has led to the discovery of geographic inequities in organ allocation. She is also interested in dancing, teaches swing dancing at the Naval Academy, and wrote her doctoral dissertation on the mathematics and robotics of dance.
Ernesto Pompeo Molmenti is an American transplant surgeon, scientist, and author. Currently practicing in Long Island, New York. He is Chief of Surgical Innovation and Vice-Chairman of the Department of Surgery at North Shore University Hospital / Northwell Health, and Professor of Surgery, Medicine, and Pediatrics at Zucker School of Medicine at Hofstra/Northwell. He is known for his description of the “Syndromic Incidence of Ovarian Cancer after Liver Transplantation, with Special Reference to Anteceding Breast Cancer,” and for the development of the vascular reconstruction technique that has been named "Molmenti technique".