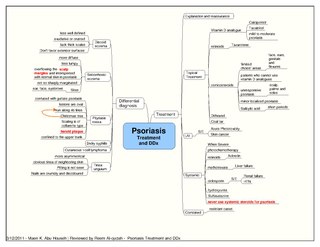
Psoriasis is a long-lasting, noncontagious autoimmune disease characterized by patches of abnormal skin. These areas are red, pink, or purple, dry, itchy, and scaly. Psoriasis varies in severity from small localized patches to complete body coverage. Injury to the skin can trigger psoriatic skin changes at that spot, which is known as the Koebner phenomenon.

Psoriatic arthritis (PsA) is a long-term inflammatory arthritis that occurs in people affected by the autoimmune disease psoriasis. The classic feature of psoriatic arthritis is swelling of entire fingers and toes with a sausage-like appearance. This often happens in association with changes to the nails such as small depressions in the nail (pitting), thickening of the nails, and detachment of the nail from the nailbed. Skin changes consistent with psoriasis frequently occur before the onset of psoriatic arthritis but psoriatic arthritis can precede the rash in 15% of affected individuals. It is classified as a type of seronegative spondyloarthropathy.
A TNF inhibitor is a pharmaceutical drug that suppresses the physiologic response to tumor necrosis factor (TNF), which is part of the inflammatory response. TNF is involved in autoimmune and immune-mediated disorders such as rheumatoid arthritis, ankylosing spondylitis, inflammatory bowel disease, psoriasis, hidradenitis suppurativa and refractory asthma, so TNF inhibitors may be used in their treatment. The important side effects of TNF inhibitors include lymphomas, infections, congestive heart failure, demyelinating disease, a lupus-like syndrome, induction of auto-antibodies, injection site reactions, and systemic side effects.
Papular mucinosis is a rare skin disease. Localized and disseminated cases are called papular mucinosis or lichen myxedematosus while generalized, confluent papular forms with sclerosis are called scleromyxedema. Frequently, all three forms are regarded as papular mucinosis. However, some authors restrict it to only mild cases. Another form, acral persistent papular mucinosis is regarded as a separate entity.

Heinrich Koebner ; was a German-Jewish dermatologist born in Breslau.
Psoriasis Area and Severity Index (PASI) is the most widely used tool for the measurement of severity of psoriasis. PASI combines the assessment of the severity of lesions and the area affected into a single score in the range 0 to 72.

The term pustular psoriasis is used for a heterogeneous group of diseases that share pustular skin characteristics.
Pruritic folliculitis of pregnancy is a skin condition that occurs in one in 3000 people, about 0.2% of cases, who are in their second to third trimester of pregnancy where the hair follicle becomes inflamed or infected, resulting in a pus filled bump. Some dermatologic conditions aside from pruritic folliculitis during pregnancy include "pruritic urticarial papules and plaques of pregnancy, atopic eruption of pregnancy, pemphigoid gestationis, intrahepatic cholestasis of pregnancy, and pustular psoriasis of pregnancy". This pruritic folliculitis of pregnancy differs from typical pruritic folliculitis; in pregnancy, it is characterized by sterile hair follicles becoming inflamed mainly involving the trunk, contrasting how typical pruritic folliculitis is mainly localized on "the upper back, shoulders, and chest." This condition was first observed after some pregnant individuals showed signs of folliculitis that were different than seen before. The inflammation was thought to be caused by hormonal imbalance, infection from bacteria, fungi, viruses or even an ingrown hair. However, there is no known definitive cause as of yet. These bumps usually begin on the belly and then spread to upper regions of the body as well as the thighs.
Impetigo herpetiformis is a form of severe pustular psoriasis occurring in pregnancy which may occur during any trimester.
Erosive pustular dermatitis of the scalp presents with pustules, erosions, and crusts on the scalp of primarily older Caucasian females, and on biopsy, has a lymphoplasmacytic infiltrate with or without foreign body giant cells and pilosebaceous atrophy.
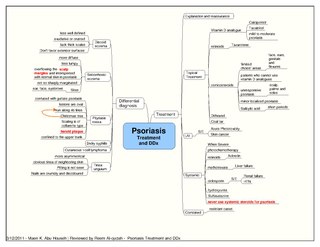
Psoriatic erythroderma represents a form of psoriasis that affects all body sites, including the face, hands, feet, nails, trunk, and extremities. This specific form of psoriasis affects 3 percent of persons diagnosed with psoriasis. First-line treatments for psoriatic erythroderma include immunosuppressive medications such as methotrexate, acitretin, or ciclosporin.

Acute generalized exanthematous pustulosis is a rare skin reaction that in 90% of cases is related to medication.

Inflammatory Linear Verrucous Epidermal Nevus is a rare disease of the skin that presents as multiple, discrete, red papules that tend to coalesce into linear plaques that follow the Lines of Blaschko. The plaques can be slightly warty (psoriaform) or scaly (eczema-like). ILVEN is caused by somatic mutations that result in genetic mosaicism. There is no cure, but different medical treatments can alleviate the symptoms.
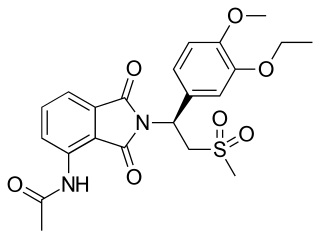
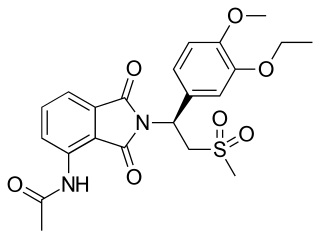
Apremilast, sold under the brand name Otezla among others, is a medication for the treatment of certain types of psoriasis and psoriatic arthritis. The drug acts as a selective inhibitor of the enzyme phosphodiesterase 4 (PDE4) and inhibits spontaneous production of TNF-alpha from human rheumatoid synovial cells. It is taken by mouth.
Stasis papillomatosis is a disease characterized by chronic congestion of the extremities, with blood circulation interrupted in a specific area of the body. A consequence of this congestion and inflammation is long-term lymphatic obstruction (lymphedema). It is also typically characterized by the appearance of numerous papules. Injuries can range from small to large plates composed of brown or pink, smooth or hyperkeratotic papules. The most typical areas where injuries occur are the back of the feet, the toes, the legs, and the area around a venous ulcer formed in the extremities, although the latter is the rarest of all. These injuries include pachydermia, lymphedema, lymphomastic verrucosis and elephantosis verrucosa. The disease can be either localized or generalized; the localized form makes up 78% of cases. Treatment includes surgical and pharmaceutical intervention; indications for partial removal include advanced fibrotic lymphedema and elephantiasis. Despite the existence of these treatments, chronic venous edema, which is a derivation of stasis papillomatosis, is only partially reversible. The skin is also affected and its partial removal may mean that the skin and the subcutaneous tissue are excised. A side effect of the procedure is the destruction of existing cutaneous lymphatic vessels. It also risks papillomatosis, skin necrosis and edema exacerbation.

Calcipotriol/betamethasone dipropionate, sold under the brand name Taclonex among others, is a fixed-dose combination medication of the synthetic vitamin D3 analog calcipotriol (also known as calcipotriene) and the synthetic corticosteroid betamethasone dipropionate for the treatment of plaque psoriasis. It is used in the form of ointment, topical suspension, gel, aerosol, and foam.
Risankizumab, sold under the brand name Skyrizi, is a humanized monoclonal antibody used for the treatment of plaque psoriasis, psoriatic arthritis, and Crohn's disease. It is designed to target interleukin 23A (IL-23A). It is given by subcutaneous injection.
Von Zumbusch (acute) generalized pustular psoriasis is the most severe form of generalized pustular psoriasis, and can be associated with life-threatening complications.
Spesolimab, sold under the brand name Spevigo, is a monoclonal antibody used for the treatment of generalized pustular psoriasis (GPP). It is an interleukin-36 receptor (IL-36R) antagonist. It is given via injection into a vein.
Joel M. Gelfand is an American dermatologist and epidemiologist at the University of Pennsylvania in Philadelphia, Pennsylvania. He currently serves as the James J. Leyden Professor in Clinical Investigation, the Vice Chair of Clinical Research, the director of the Psoriasis and Phototherapy Treatment Center, and the medical director of the Clinical Studies Unit in the Department of Dermatology at the Perelman School of Medicine at the University of Pennsylvania. He studies systemic comorbidities of psoriasis and much of his research has centered on the connection between cardiovascular disease and psoriasis.