Related Research Articles

A tendon or sinew is a tough, high-tensile-strength band of dense fibrous connective tissue that connects muscle to bone. It is able to efficiently transmit the mechanical forces of muscle contraction to the skeletal system without sacrificing its ability to withstand significant amounts of tension.

In biology, the extracellular matrix (ECM) is a three-dimensional network consisting of extracellular macromolecules and minerals, such as collagen, enzymes, glycoproteins and hydroxyapatite that provide structural and biochemical support to surrounding cells. Because multicellularity evolved independently in different multicellular lineages, the composition of ECM varies between multicellular structures; however, cell adhesion, cell-to-cell communication and differentiation are common functions of the ECM.
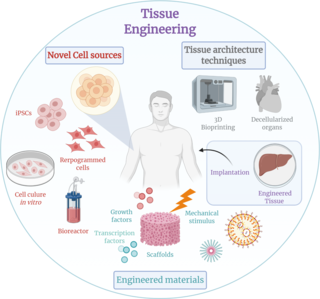
Tissue engineering is a biomedical engineering discipline that uses a combination of cells, engineering, materials methods, and suitable biochemical and physicochemical factors to restore, maintain, improve, or replace different types of biological tissues. Tissue engineering often involves the use of cells placed on tissue scaffolds in the formation of new viable tissue for a medical purpose but is not limited to applications involving cells and tissue scaffolds. While it was once categorized as a sub-field of biomaterials, having grown in scope and importance it can be considered as a field in its own.

Ultrastructure is the architecture of cells and biomaterials that is visible at higher magnifications than found on a standard optical light microscope. This traditionally meant the resolution and magnification range of a conventional transmission electron microscope (TEM) when viewing biological specimens such as cells, tissue, or organs. Ultrastructure can also be viewed with scanning electron microscopy and super-resolution microscopy, although TEM is a standard histology technique for viewing ultrastructure. Such cellular structures as organelles, which allow the cell to function properly within its specified environment, can be examined at the ultrastructural level.

Wound healing refers to a living organism's replacement of destroyed or damaged tissue by newly produced tissue.

Hyaluronic acid, also called hyaluronan, is an anionic, nonsulfated glycosaminoglycan distributed widely throughout connective, epithelial, and neural tissues. It is unique among glycosaminoglycans as it is non-sulfated, forms in the plasma membrane instead of the Golgi apparatus, and can be very large: human synovial HA averages about 7 million Da per molecule, or about 20,000 disaccharide monomers, while other sources mention 3–4 million Da.
Chin augmentation using surgical implants can alter the underlying structure of the face, providing better balance to the facial features. The specific medical terms mentoplasty and genioplasty are used to refer to the reduction and addition of material to a patient's chin. This can take the form of chin height reduction or chin rounding by osteotomy, or chin augmentation using implants. Improving the facial balance is commonly performed by enhancing the Chin using an implant inserted through the mouth. The goal is to provide a suitable projection of the chin as well as the correct height of the chin which is in balance with the other facial features.

Tendinitis/tendonitis is inflammation of a tendon, often involving torn collagen fibers. A bowed tendon is a horseman's term for a tendon after a horse has sustained an injury that causes swelling in one or more tendons creating a "bowed" appearance.

An artificial heart valve is a one-way valve implanted into a person's heart to replace a heart valve that is not functioning properly. Artificial heart valves can be separated into three broad classes: mechanical heart valves, bioprosthetic tissue valves and engineered tissue valves.

A biomaterial is a substance that has been engineered to interact with biological systems for a medical purpose, either a therapeutic or a diagnostic one. As a science, biomaterials is about fifty years old. The study of biomaterials is called biomaterials science or biomaterials engineering. It has experienced steady and strong growth over its history, with many companies investing large amounts of money into the development of new products. Biomaterials science encompasses elements of medicine, biology, chemistry, tissue engineering and materials science.

A foreign body reaction (FBR) is a typical tissue response to a foreign body within biological tissue. It usually includes the formation of a foreign body granuloma. Tissue-encapsulation of an implant is an example, as is inflammation around a splinter. Foreign body granuloma formation consists of protein adsorption, macrophages, multinucleated foreign body giant cells, fibroblasts, and angiogenesis. It has also been proposed that the mechanical property of the interface between an implant and its surrounding tissues is critical for the host response.
A nerve guidance conduit is an artificial means of guiding axonal regrowth to facilitate nerve regeneration and is one of several clinical treatments for nerve injuries. When direct suturing of the two stumps of a severed nerve cannot be accomplished without tension, the standard clinical treatment for peripheral nerve injuries is autologous nerve grafting. Due to the limited availability of donor tissue and functional recovery in autologous nerve grafting, neural tissue engineering research has focused on the development of bioartificial nerve guidance conduits as an alternative treatment, especially for large defects. Similar techniques are also being explored for nerve repair in the spinal cord but nerve regeneration in the central nervous system poses a greater challenge because its axons do not regenerate appreciably in their native environment.
Acellular dermis is a type of biomaterial derived from processing human or animal tissues to remove cells and retain portions of the extracellular matrix (ECM). These materials are typically cell-free, distinguishing them from classical allografts and xenografts, can be integrated or incorporated into the body, and have been FDA approved for human use for more than 10 years in a wide range of clinical indications.

Biomaterials are materials that are used in contact with biological systems. Biocompatibility and applicability of surface modification with current uses of metallic, polymeric and ceramic biomaterials allow alteration of properties to enhance performance in a biological environment while retaining bulk properties of the desired device.
Dermal fibroblasts are cells within the dermis layer of skin which are responsible for generating connective tissue and allowing the skin to recover from injury. Using organelles, dermal fibroblasts generate and maintain the connective tissue which unites separate cell layers. Furthermore, these dermal fibroblasts produce the protein molecules including laminin and fibronectin which comprise the extracellular matrix. By creating the extracellular matrix between the dermis and epidermis, fibroblasts allow the epithelial cells of the epidermis to affix the matrix, thereby allowing the epidermal cells to effectively join together to form the top layer of the skin.
The Network of Excellence for Functional Biomaterials (NFB) is a multidisciplinary research centre which hosts over sixty biologists, chemists, scientists, engineers and clinicians. It is based at the National University of Ireland, Galway, and is directed by Professor Abhay Pandit.
Decellularization of porcine heart valves is the removal of cells along with antigenic cellular elements by either physical or chemical decellularization of the tissue. This decellularized valve tissue provides a scaffold with the remaining extracellular matrix (ECM) that can then be used for tissue engineering and valve replacement in humans inflicted with valvular disease. Decellularized biological valves have potential benefit over conventional valves through decreased calcification which is thought to be an immuno-inflammatory response initiated by the recipient.

Surgical mesh is a loosely woven sheet which is used as either a permanent or temporary support for organs and other tissues during surgery. Surgical mesh is created from both inorganic and biological materials and is used in a variety of surgeries. Though hernia repair surgery is the most common application, it can also be used for reconstructive work, such as in pelvic organ prolapse.
Nasal chondrocytes (NC) are present in the hyaline cartilage of the nasal septum, and in fact are the only cell type within the tissue. Similar to chondrocytes present in articular cartilage, NC express extracellular matrix proteins such as glycosaminoglycans and collagen.
Tissue engineered heart valves (TEHV) offer a new and advancing proposed treatment of creating a living heart valve for people who are in need of either a full or partial heart valve replacement. Currently, there are over a quarter of a million prosthetic heart valves implanted annually, and the number of patients requiring replacement surgeries is only suspected to rise and even triple over the next fifty years. While current treatments offered such as mechanical valves or biological valves are not deleterious to one's health, they both have their own limitations in that mechanical valves necessitate the lifelong use of anticoagulants while biological valves are susceptible to structural degradation and reoperation. Thus, in situ tissue engineering of heart valves serves as a novel approach that explores the use creating a living heart valve composed of the host's own cells that is capable of growing, adapting, and interacting within the human body's biological system.
References
- ↑ Zerris et al. Journal of Biomedical Materials Research Part B, Volume 83B Issue 2, Pages 580 - 588, 2007 Article
- 1 2 3 4 Cornwell, Landsman, James. Extracellular Matrix Biomaterials for Soft Tissue Repair. Clin Podiatr Med Surg 26 (2009) 507–523 Article
- ↑ Valentin JE, Badylak JS, McCabe GP, et al. Extracellular matrix bioscaffolds for orthopaedic applications. A comparative histologic study. J Bone Joint Surg Am 2006;88(12):2673–86. Article Archived 2009-08-12 at the Wayback Machine
- ↑ Hwang K, Hwang JH, et al. Experimental study of autologous cartilage, acellular cadaveric dermis, lyophilized bovine pericardium, and irradiated bovine tendon: applicability to nasal tip plasty. J Craniofac Surg 2007;18(3):551–8 Article on Pubmed
- ↑ SurgiMend, TEI Biosciences Inc. Website Archived 2016-07-10 at the Wayback Machine
- ↑ TissueMend, Stryker Orthopaedics Website
- ↑ Durepair, Medtronic Website