In 2017, ICDDR,B won the Conrad N. Hilton Humanitarian Prize with $2 million in prize money in recognition [8] of the institute's innovative approach to solving global health issues impacting the world's most impoverished communities. In 2016, former UN Secretary-General Ban Ki-moon noted [9] that ICDDR,B's innovations are directly contributing to sustainable development, helping reduce infant, child and maternal mortality significantly in Bangladesh and beyond.
Timeline of Innovations and achievements
1960: Cholera Research Laboratory begins.
1963: Population surveillance – the world's longest running field site starts in Matlab Bazaar. [11]
1966: Cholera fatality reduced to less than 1%.
1967: Work leading to the development of oral rehydration therapy begins.
1969: Relationship between breastfeeding and menstruation resumption is demonstrated.
1974: Tetanus toxoid vaccine recommended for pregnant women, reducing neonatal mortality by 30%.
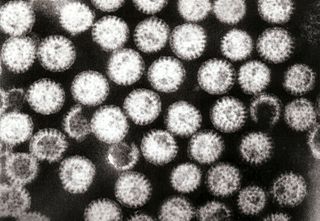
1978: Rotavirus identified as the most common cause of diarrhoea in infants in Bangladesh, and as highest priority for new vaccines.
1982: Rice-based ORS shown to be fully effective alternative to glucose-based ORS and preferred for routine use at ICDDR,B.
1982: Matlab Maternal Child Health and Family Planning project shares its success in lowering national fertility rates with the Government of Bangladesh.
1983: Epidemic Control and Preparedness Programme begins.
1984: Full Expanded Programme on Immunization data is validated (and begins). Benefit of measles vaccine demonstrated, leading to inclusion in EPI.
1985: Cholera vaccine trial launched.
1988: Treatment of, and research into, acute respiratory infections/pneumonia begins.
1989: Matlab record keeping system, specially adapted for Government use, extended to the national family planning programme.
1993: New Vibrio cholerae 0139 (Bengal strain) identified and characterised by ICDDR,B.
1994: ICDDR,B epidemic response team goes to Goma, Zaire to assist cholera-stricken Rwandan refugees and helps reduce case fatality rate from as high as 49% to less than 1%.
1995: Maternal immunisation with pneumococcal vaccine shown likely to protect infants up to 22 weeks.
1998: HIV sero-surveillance begins in Bangladesh on behalf of Ministry of Health and Family Welfare, Government of Bangladesh.
1999: Protocolized Management of Severely Malnourished Children decreases case fatality from 20% to less than 5%. Published in Lancet.
2000: ICDDR,B assists Government of Bangladesh with control of major dengue epidemic in Dhaka.
2000: International, peer-reviewed and indexed ICDDR,B journal is renamed Journal of Health, Population, and Nutrition.
2001: Studies on violence against women in Bangladesh are initiated.
2001: ICDDR,B opens the first tuberculosis laboratory in Bangladesh.
2001: Oral cholera vaccine, tested at ICDDR,B, is approved for use by WHO.
2001: Studies on the effects of arsenic on health begin.
2002: ICDDR,B studies establish that zinc treatment of diarrhoea reduces under-5 mortality by 50%.
2002: First HIV voluntary counselling and testing unit in Bangladesh opens at ICDDR,B.
2003: New research programmes on HIV/AIDS and Poverty & Health.
2004: Studies on preventing high levels of childhood drowning begin.
2005: ICDDR,B team assists in post-tsunami health needs assessment in Sri Lanka.
2006: Dispersible zinc tablets launched through unique public-private partnership in national scale-up to treat diarrhoea in children under five years.
2006: Studies on abortion and menstrual regulation initiated.
2007: Oral cholera vaccine Dukoral, tested at Matlab in 1985, launched in Bangladesh.
2008: Introduce SHEBA (an integrated Hospital Management System) and start the journey as a paperless hospital
2009: ICDDR,B opens a ward for ARI (Swine Flu) patients.
2010: ICDDR,B celebrates 50 years of operations. Sends teams to combat deadly cholera outbreaks in Pakistan and Haiti. Research team discovers and characterise the "TLC phage" which changes the chromosomal sequence of the cholera bacterium, enabling incoming toxigenic CTX phage genome to be incorporated and transforming a harmless strain of V. cholerae to a dangerous killer. Issued its first patent from the Director of United States Patent and Trademark Office (United States Patent US7638271) for inventing a new diagnostic method for tuberculosis, called Antibodies from lymphocyte secretions or ALS.
2011: "Continuum of Care" (a concept [12] involving a system that guides and tracks patients over time through a comprehensive array of health services) approach achieves 36% drop in perinatalmortality.
2014: Oral cholera vaccine in Bangladesh was found [13] to have significant impact on cholera incidence when delivered through Bangladesh's existing immunisation infrastructure.
2015: ICDDR,B published a three-year strategic plan [14] 2015–2018, aiming to achieve broader objectives by developing a greater international focus, promoting the growth of South-South collaborations and increasing engagement with the private sector.
2016: Former UN Secretary-General Ban Ki-moon acknowledged [9] that ICDDR,B interventions are directly contributing to sustainable development, which helped to significantly reduce infant, child and maternal mortality in Bangladesh and beyond.
2017: ICDDR,B wins the 2017 Conrad N. Hilton Humanitarian Prize [15] for its commitment to solving key public health problems facing the world's most vulnerable through innovative scientific research since 1960.