This article has multiple issues. Please help improve it or discuss these issues on the talk page . (Learn how and when to remove these template messages)
|
Ian Brockington (born 1935) is a British psychiatrist.
This article has multiple issues. Please help improve it or discuss these issues on the talk page . (Learn how and when to remove these template messages)
|
Ian Brockington (born 1935) is a British psychiatrist.
Ian Fraser Brockington was educated at Winchester College and Gonville and Caius College Cambridge. He received his medical training at Manchester University. [1] His doctoral thesis was on 'Heart muscle disease'. [2]
He spent four years in Ibadan, Nigeria, alternating with training posts at the Royal Postgraduate Medical School with Professor Goodwin; [1] this resulted in a number of papers on African heart diseases.[ citation needed ]
On his return he switched to psychiatry, with training at the Maudsley Hospital. He worked with the late Robert Evan Kendell on schizoaffective disorders and wrote a series of papers on the nosology of the psychoses. As Senior Lecturer at the Victoria University of Manchester he developed an interest in mother–infant psychiatry. After visiting professorships in Chicago and St Louis, he was appointed to the Chair of Psychiatry at the University of Birmingham. There he developed a community-based clinical service for mothers, backed by an inpatient mother and baby unit and day hospital. He had sabbaticals as Cottman Fellow in Monash University, and locum tenens consultant at the mother and baby unit in Christchurch, New Zealand.[ citation needed ]
He helped to found, and was the first President of, the Marcé Society, and founded the Section on Women's Mental Health in the World Psychiatric Association. He has established three anonymous patient panels: Action on Puerperal Psychosis, Action on Menstrual Psychosis, and Action on Bonding Disorders.
Since his retirement from clinical and university work in 2001, he had visiting professorships in Nagoya (with Professor Honjo) and Kumamoto (with Professor Kitamura).[ citation needed ]
He chaired a World Psychiatric Association taskforce on child protection. [3]
With a hobby of bookbinding, he established Eyry Press. [4] He has written six monographs on the psychiatry of childbearing, four of which he published himself.
Menstrual psychosis is a medical condition that Brockinton proposed for a periodic display of psychosis with acute onset in a particular phase of the menstrual cycle. [5] It is proposed as a form of severe mental illness, whose clinical features resemble those of the common form of postpartum psychosis; since most cases are considered to belong to the bipolar disorder spectrum, it is not a "disease in its own right". [5] According to Brockington, between the early 1800s and the early 2000s, 27 confirmed cases and nearly 200 possible cases of menstruation and brief psychotic episdoes happening at the same time have been reported in the medical literature. [6] Episodes of menstrual psychosis have a sudden onset in a previously asymptomatic person, and are usually of brief duration, with full recovery. [5] In most patients, Brockington states that menstrual psychosis is a self-limiting disorder, affecting only a small proportion of the 400 menstrual cycles in a woman’s life. [7]
Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior that is inappropriate for a given situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Psychosis can have serious adverse outcomes.

Schizophrenia is a mental disorder characterized by continuous or relapsing episodes of psychosis. Major symptoms include hallucinations, delusions, and disorganized thinking. Other symptoms include social withdrawal, decreased emotional expression, and apathy. Symptoms typically develop gradually, begin during young adulthood, and in many cases never become resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a psychiatric history that includes the person's reported experiences, and reports of others familiar with the person. To be diagnosed with schizophrenia, symptoms and functional impairment need to be present for six months (DSM-5) or one month (ICD-11). Many people with schizophrenia have other mental disorders, especially substance use disorders, depressive disorders, anxiety disorders, and obsessive–compulsive disorder.
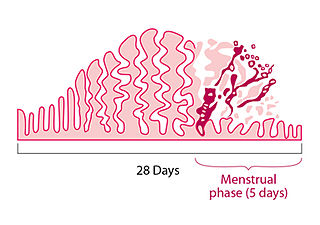
Menstruation is the regular discharge of blood and mucosal tissue from the inner lining of the uterus through the vagina. The menstrual cycle is characterized by the rise and fall of hormones. Menstruation is triggered by falling progesterone levels and is a sign that pregnancy has not occurred.
Premenstrual syndrome (PMS) is a disruptive set of emotional and physical symptoms that regularly occur in the one to two weeks before the start of each menstrual period. Symptoms resolve around the time menstrual bleeding begins. Different women experience different symptoms. Premenstrual syndrome commonly produces one or more physical, emotional, or behavioral symptoms, that resolve with menses. The range of symptoms is wide, and most commonly are breast tenderness, bloating, headache, mood swings, depression, anxiety, anger, and irritability. To be diagnosed as PMS, rather than a normal discomfort of the menstrual cycle, these symptoms must interfere with daily living, during two menstrual cycles of prospective recording. These symptoms are nonspecific and are seen in women without PMS. Often PMS-related symptoms are present for about six days. An individual's pattern of symptoms may change over time. PMS does not produce symptoms during pregnancy or following menopause.
Schizoaffective disorder is a mental disorder characterized by abnormal thought processes and an unstable mood. This diagnosis requires symptoms of both schizophrenia and a mood disorder: either bipolar disorder or depression. The main criterion is the presence of psychotic symptoms for at least two weeks without any mood symptoms. Schizoaffective disorder can often be misdiagnosed when the correct diagnosis may be psychotic depression, bipolar I disorder, schizophreniform disorder, or schizophrenia. This is a problem as treatment and prognosis differ greatly for most of these diagnoses.
Richard Bentall is a Professor of Clinical Psychology at the University of Sheffield in the UK.
A syndrome is a set of medical signs and symptoms which are correlated with each other and often associated with a particular disease or disorder. The word derives from the Greek σύνδρομον, meaning "concurrence". When a syndrome is paired with a definite cause this becomes a disease. In some instances, a syndrome is so closely linked with a pathogenesis or cause that the words syndrome, disease, and disorder end up being used interchangeably for them. This substitution of terminology often confuses the reality and meaning of medical diagnoses. This is especially true of inherited syndromes. About one third of all phenotypes that are listed in OMIM are described as dysmorphic, which usually refers to the facial gestalt. For example, Down syndrome, Wolf–Hirschhorn syndrome, and Andersen–Tawil syndrome are disorders with known pathogeneses, so each is more than just a set of signs and symptoms, despite the syndrome nomenclature. In other instances, a syndrome is not specific to only one disease. For example, toxic shock syndrome can be caused by various toxins; another medical syndrome named as premoter syndrome can be caused by various brain lesions; and premenstrual syndrome is not a disease but simply a set of symptoms.
Premenstrual dysphoric disorder (PMDD) is a mood disorder characterized by emotional, cognitive, and physical symptoms. PMDD causes significant distress or impairment in menstruating women during the luteal phase of the menstrual cycle. The symptoms occur in the luteal phase, improve within a few days after the onset of menses, and are minimal or absent in the week after menses. PMDD has a profound impact on a person's quality of life and dramatically increases the risk of suicidal ideation and even suicide attempts. Many women of reproductive age experience discomfort or mild mood changes prior to menstruation. However, 5-8% experience severe premenstrual syndrome causing significant distress or functional impairment. Within this population of reproductive age, some will meet the criteria for PMDD.
Psychoneuroendocrinology is the clinical study of hormone fluctuations and their relationship to human behavior. It may be viewed from the perspective of psychiatry, where in certain mood disorders, there are associated neuroendocrine or hormonal changes affecting the brain. It may also be viewed from the perspective of endocrinology, where certain endocrine disorders can be associated with negative health outcomes and psychiatric illness. Brain dysfunctions associated with the hypothalamus-pituitary-adrenal axis HPA axis can affect the endocrine system, which in turn can result in physiological and psychological symptoms. This complex blend of psychiatry, psychology, neurology, biochemistry, and endocrinology is needed to comprehensively understand and treat symptoms related to the brain, endocrine system (hormones), and psychological health..
Oneiroid syndrome (OS) is a condition involving dream-like disturbances of one's consciousness by vivid scenic hallucinations, accompanied by catatonic symptoms (either catatonic stupor or excitement), delusions, or psychopathological experiences of a kaleidoscopic nature. The term is from Ancient Greek "ὄνειρος" (óneiros, meaning "dream") and "εἶδος" (eîdos, meaning "form, likeness"; literally dream-like / oneiric or oniric, sometimes called "nightmare-like"). It is a common complication of catatonic schizophrenia, although it can also be caused by other mental disorders. The dream-like experiences are vivid enough to seem real to the patient. OS is distinguished from delirium by the fact that the imaginative experiences of patients always have an internal projection. This syndrome is hardly mentioned in standard psychiatric textbooks, possibly because it is not listed in DSM.
Pierre Flor-Henry is a Canadian psychiatrist, researcher, lecturer, and professor. His most important initial contribution was the demonstration in the study of epileptic psychosis, that schizophrenia relates to left and manic-depressive states relate to right hemisphere epilepsies.
Brief psychotic disorder — according to the classifications of mental disorders DSM-IV-TR and DSM-5 — is a psychotic condition involving the sudden onset of at least one psychotic symptom lasting 1 day to 1 month, often accompanied by emotional turmoil. Remission of all symptoms is complete with patients returning to the previous level of functioning. It may follow a period of extreme stress including the loss of a loved one. Most patients with this condition under DSM-5 would be classified as having acute and transient psychotic disorders under ICD-10. Prior to DSM-IV, this condition was called "brief reactive psychosis." This condition may or may not be recurrent, and it should not be caused by another condition.

Postpartum psychosis(PPP), also known as puerperal psychosis or peripartum psychosis, involves the abrupt onset of psychotic symptoms shortly following childbirth, typically within two weeks of delivery but less than 4 weeks postpartum. PPP is a condition currently represented under "Brief Psychotic Disorder" in the Diagnostic and Statistical Manual of Mental Disorders, Volume V (DSM-V). Symptoms may include delusions, hallucinations, disorganized speech (e.g, incoherent speech), and/or abnormal motor behavior (e.g., catatonia). Other symptoms frequently associated with PPP include confusion, disorganized thought, severe difficulty sleeping, variations of mood disorders (including depression, agitation, mania, or a combination of the above), as well as cognitive features such as consciousness that comes and goes (waxing and waning) or disorientation.
A postpartum disorder or puerperal disorder is a disease or condition which presents primarily during the days and weeks after childbirth called the postpartum period. The postpartum period can be divided into three distinct stages: the initial or acute phase, 6–12 hours after childbirth; subacute postpartum period, which lasts two to six weeks, and the delayed postpartum period, which can last up to six months. In the subacute postpartum period, 87% to 94% of women report at least one health problem. Long term health problems are reported by 31% of women.
Psychiatric disorders of childbirth, as opposed to those of pregnancy or the postpartum period, are psychiatric complications that develop during or immediately following childbirth. Despite modern obstetrics and pain control, these disorders are still observed. Most often, psychiatric disorders of childbirth present as delirium, stupor, rage, acts of desperation, or neonaticide. These psychiatric complications are rarely seen in patients under modern medical supervision. However, care disparities between Europe, North America, Australia, Japan, and other countries with advanced medical care and the rest of the world persist. The wealthiest nations represent 10 million births each year out of the world's total of 135 million. These nations have a maternal mortality rate (MMR) of 6–20/100,000. Poorer nations with high birth rates can have an MMR more than 100 times higher. In Africa, India & South East Asia, as well as Latin America, these complications of parturition may still be as prevalent as they have been throughout human history.
The word schizophrenia was coined by the Swiss psychiatrist Eugen Bleuler in 1908, and was intended to describe the separation of function between personality, thinking, memory, and perception. He introduced the term on 24 April 1908 in a lecture given at a psychiatric conference in Berlin and in a publication that same year. Bleuler later expanded his new disease concept into a monograph in 1911, which was finally translated into English in 1950.

The Kraepelinian dichotomy is the division of the major endogenous psychoses into the disease concepts of dementia praecox, which was reformulated as schizophrenia by Eugen Bleuler by 1908, and manic-depressive psychosis, which has now been reconceived as bipolar disorder. This division was formally introduced in the sixth edition of Emil Kraepelin's psychiatric textbook Psychiatrie. Ein Lehrbuch für Studirende und Aerzte, published in 1899. It has been highly influential on modern psychiatric classification systems, the DSM and ICD, and is reflected in the taxonomic separation of schizophrenia from affective psychosis. However, there is also a diagnosis of schizoaffective disorder to cover cases that seem to show symptoms of both.
Unitary psychosis (Einheitspsychose) refers to the 19th-century belief prevalent in German psychiatry until the era of Emil Kraepelin that all forms of psychosis were surface variations of a single underlying disease process. According to this model, there were no distinct disease entities in psychiatry but only varieties of a single universal madness and the boundaries between these variants were fluid. The prevalence of the concept in Germany during the mid-19th century can be understood in terms of a general resistance to Cartesian dualism and faculty psychology as expressed in Naturphilosophie and other Romantic doctrines that emphasised the unity of body, mind and spirit.
Menstrual migraine is term used to describe both true menstrual migraines and menstrually related migraines. About 7%–14% of women have migraines only at the time of menstruation, these are called true menstrual migraines. Most female migraneurs experience migraine attacks throughout the menstruation cycle with an increased number perimenstrually, these are referred to as menstrually related or menstrually triggered migraine.
The malaria therapy is a medical procedure of treating diseases using artificial injection of malaria parasites. It is a type of pyrotherapy by which high fever is induced to stop or eliminate symptoms of certain diseases. In malaria therapy, malarial parasites (Plasmodium) are specifically used to cause fever, and an elevated body temperature reduces the symptoms of or cure the diseases. As the primary disease is treated, the malaria is then cured using antimalarial drugs. The method was developed by Austrian physician Julius Wagner-Jauregg in 1917 for the treatment of neurosyphilis for which he received the 1927 Nobel Prize in Physiology or Medicine.