The kidneys are two reddish-brown bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about 12 centimetres in length. They receive blood from the paired renal arteries; blood exits into the paired renal veins. Each kidney is attached to a ureter, a tube that carries excreted urine to the bladder.

Nephrology is a specialty of adult internal medicine and pediatric medicine that concerns the study of the kidneys, specifically normal kidney function and kidney disease, the preservation of kidney health, and the treatment of kidney disease, from diet and medication to renal replacement therapy. The word “renal” is an adjective meaning “relating to the kidneys”, and its roots are French or late Latin. Whereas according to some opinions, "renal" and "nephro" should be replaced with "kidney" in scientific writings such as "kidney medicine" or "kidney replacement therapy", other experts have advocated preserving the use of renal and nephro as appropriate including in "nephrology" and "renal replacement therapy", respectively.

In medicine, dialysis is the process of removing excess water, solutes, and toxins from the blood in people whose kidneys can no longer perform these functions naturally. This is referred to as renal replacement therapy. The first successful dialysis was performed in 1943.
The excretory system is a passive biological system that removes excess, unnecessary materials from the body fluids of an organism, so as to help maintain internal chemical homeostasis and prevent damage to the body. The dual function of excretory systems is the elimination of the waste products of metabolism and to drain the body of used up and broken down components in a liquid and gaseous state. In humans and other amniotes most of these substances leave the body as urine and to some degree exhalation, mammals also expel them through sweating.

Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys are functioning at less than 15% of normal levels. Kidney failure is classified as either acute kidney failure, which develops rapidly and may resolve; and chronic kidney failure, which develops slowly and can often be irreversible. Symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications of acute and chronic failure include uremia, high blood potassium, and volume overload. Complications of chronic failure also include heart disease, high blood pressure, and anemia.
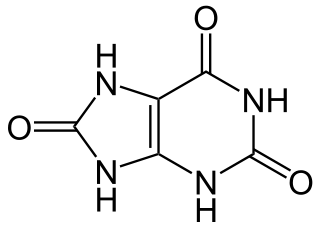
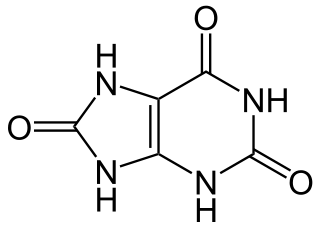
Hyperuricaemia or hyperuricemia is an abnormally high level of uric acid in the blood. In the pH conditions of body fluid, uric acid exists largely as urate, the ion form. Serum uric acid concentrations greater than 6 mg/dL for females, 7 mg/dL for men, and 5.5 mg/dL for youth are defined as hyperuricemia. The amount of urate in the body depends on the balance between the amount of purines eaten in food, the amount of urate synthesised within the body, and the amount of urate that is excreted in urine or through the gastrointestinal tract. Hyperuricemia may be the result of increased production of uric acid, decreased excretion of uric acid, or both increased production and reduced excretion.

Kidney disease, or renal disease, technically referred to as nephropathy, is damage to or disease of a kidney. Nephritis is an inflammatory kidney disease and has several types according to the location of the inflammation. Inflammation can be diagnosed by blood tests. Nephrosis is non-inflammatory kidney disease. Nephritis and nephrosis can give rise to nephritic syndrome and nephrotic syndrome respectively. Kidney disease usually causes a loss of kidney function to some degree and can result in kidney failure, the complete loss of kidney function. Kidney failure is known as the end-stage of kidney disease, where dialysis or a kidney transplant is the only treatment option.

Chronic kidney disease (CKD) is a type of kidney disease in which there is gradual loss of kidney function over a period of months to years. Initially there are generally no symptoms; later, symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications can relate to hormonal dysfunction of the kidneys and include high blood pressure, bone disease, and anemia. Additionally CKD patients have markedly increased cardiovascular complications with increased risks of death and hospitalization.

Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids. Metabolic acidosis can lead to acidemia, which is defined as arterial blood pH that is lower than 7.35. Acidemia and acidosis are not mutually exclusive – pH and hydrogen ion concentrations also depend on the coexistence of other acid-base disorders; therefore, pH levels in people with metabolic acidosis can range from low, normal, to high.

A high-protein diet is a diet in which 20% or more of the total daily calories comes from protein. Most high protein diets are high in saturated fat and severely restrict intake of carbohydrates.
Protein toxicity is the effect of the buildup of protein metabolic waste compounds, like urea, uric acid, ammonia, and creatinine. Protein toxicity has many causes, including urea cycle disorders, genetic mutations, excessive protein intake, and insufficient kidney function, such as chronic kidney disease and acute kidney injury. Symptoms of protein toxicity include unexplained vomiting and loss of appetite. Untreated protein toxicity can lead to serious complications such as seizures, encephalopathy, further kidney damage, and even death.
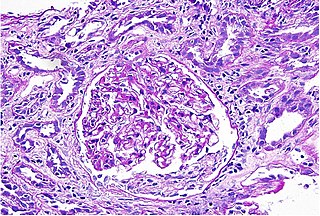
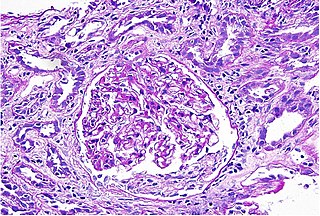
Interstitial nephritis, also known as tubulointerstitial nephritis, is inflammation of the area of the kidney known as the renal interstitium, which consists of a collection of cells, extracellular matrix, and fluid surrounding the renal tubules. In addition to providing a scaffolding support for the tubular architecture, the interstitium has been shown to participate in the fluid and electrolyte exchange as well as endocrine functions of the kidney.

Robert Provenzano is an American nephrologist. He is also an Associate Clinical Professor of Medicine at Wayne State University School of Medicine.
T. Alp Ikizler is a nephrologist, currently holding the Catherine McLaughlin Hakim chair in Medicine at Vanderbilt University School of Medicine, where he does clinical work and heads a research lab. Born in Istanbul, Turkey, he received his M.D. from the Istanbul University Faculty of Medicine.
Nathan W. Levin is an American physician and founder of the Renal Research Institute, LLC., a research institute dedicated to improving the outcomes of patients with kidney disease, particularly those requiring dialysis. Levin is one of the most prominent and renowned figures in clinical nephrology as well as nephrology research. He has authored multiple book chapters and over 350 peer-reviewed publications, including articles in leading journals such as Nature, the New England Journal of Medicine, and The Lancet.
Calcium acetate/magnesium carbonate is a fixed-dose combination drug that contains 110 mg calcium and 60 mg magnesium ions and is indicated as a phosphate binder for dialysis patients suffering from hyperphosphataemia. It is registered by Fresenius Medical Care under the trade names Renepho (Belgium) and OsvaRen.
Joel D. Kopple is an American professor, physician, and clinical investigator in medicine, nephrology, nutrition, and public health. He is professor at David Geffen UCLA School of Medicine and UCLA Fielding School of Public Health. He served from 1982 to 2007 as the chief of the Division of Nephrology and Hypertension at Harbor-UCLA Medical Center. He is also known as the father of the field of Renal Nutrition.
Kamyar Kalantar-Zadeh is an Iranian-American physician doing research in nephrology, kidney dialysis, nutrition, and epidemiology. He is best known as a specialist in kidney disease nutrition and chronic kidney disease and for his hypothesis about the longevity of individuals with chronic disease states, also known as reverse epidemiology including obesity paradox. According to this hypothesis, obesity or hypercholesterolemia may counterintuitively be protective and associated with greater survival in certain groups of people, such as elderly individuals, dialysis patients, or those with chronic disease states and wasting syndrome (cachexia), whereas normal to low body mass index or normal values of serum cholesterol may be detrimental and associated with worse mortality. Kalantar-Zadeh is also known for his expertise in kidney dialysis therapy, including incremental dialysis, as well as renal nutrition. He is the brother of Kourosh Kalantar-zadeh, who an Australian scientist involved in research in the fields of materials sciences, nanotechnology, and transducers.

Carmine Zoccali is an Italian nephrologist and a clinical investigator. He has contributed to research in several fields, most notably hypertension and cardiovascular complications in chronic kidney disease (CKD), CKD progression and clinical epidemiology of kidney diseases at large. He is known for his studies on cardiovascular risk in CKD and dialysis patients. He was among the earliest investigators that focused on the relevance of endothelial dysfunction and inflammation for the high risk of cardiovascular disease in these populations. In this research area, he was the first to link endogenous inhibitors of the nitric oxide system with death and cardiovascular disease. and the first to document a relationship between sympathetic over-activity and these outcomes Dr Zoccali is a practicing specialist in Nephrology, with a national qualification for the full professorship in Nephrology. He is also a specialist in hypertension, certified by the European Society of Hypertension (ESH).
Kidney ischemia is a disease with a high morbidity and mortality rate. Blood vessels shrink and undergo apoptosis which results in poor blood flow in the kidneys. More complications happen when failure of the kidney functions result in toxicity in various parts of the body which may cause septic shock, hypovolemia, and a need for surgery. What causes kidney ischemia is not entirely known, but several pathophysiology relating to this disease have been elucidated. Possible causes of kidney ischemia include the activation of IL-17C and hypoxia due to surgery or transplant. Several signs and symptoms include injury to the microvascular endothelium, apoptosis of kidney cells due to overstress in the endoplasmic reticulum, dysfunctions of the mitochondria, autophagy, inflammation of the kidneys, and maladaptive repair.