Related Research Articles
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs in an attempt to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same sex and opposite sex partners so long as the HIV-positive partner maintains an undetectable viral load.
The spread of HIV/AIDS has affected millions of people worldwide; AIDS is considered a pandemic. The World Health Organization (WHO) estimated that in 2016 there were 36.7 million people worldwide living with HIV/AIDS, with 1.8 million new HIV infections per year and 1 million deaths due to AIDS. Misconceptions about HIV and AIDS arise from several different sources, from simple ignorance and misunderstandings about scientific knowledge regarding HIV infections and the cause of AIDS to misinformation propagated by individuals and groups with ideological stances that deny a causative relationship between HIV infection and the development of AIDS. Below is a list and explanations of some common misconceptions and their rebuttals.

Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When the brain is infected, symptoms include headache, fever, neck pain, nausea and vomiting, light sensitivity and confusion or changes in behaviour. It can also affect other parts of the body including skin, where it may appear as several fluid-filled nodules with dead tissue.
Following infection with HIV-1, the rate of clinical disease progression varies between individuals. Factors such as host susceptibility, genetics and immune function, health care and co-infections as well as viral genetic variability may affect the rate of progression to the point of needing to take medication in order not to develop AIDS.
Immune reconstitution inflammatory syndrome (IRIS) is a condition seen in some cases of AIDS or immunosuppression, in which the immune system begins to recover, but then responds to a previously acquired opportunistic infection with an overwhelming inflammatory response that paradoxically makes the symptoms of infection worse.
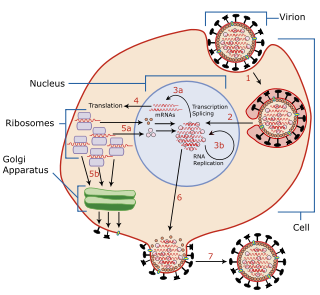
Virus latency is the ability of a pathogenic virus to lie dormant within a cell, denoted as the lysogenic part of the viral life cycle. A latent viral infection is a type of persistent viral infection which is distinguished from a chronic viral infection. Latency is the phase in certain viruses' life cycles in which, after initial infection, proliferation of virus particles ceases. However, the viral genome is not eradicated. The virus can reactivate and begin producing large amounts of viral progeny without the host becoming reinfected by new outside virus, and stays within the host indefinitely.

Human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV), a retrovirus. Following initial infection a person may not notice any symptoms, or may experience a brief period of influenza-like illness. Typically, this is followed by a prolonged period with no symptoms. If the infection progresses, it interferes more with the immune system, increasing the risk of developing common infections such as tuberculosis, as well as other opportunistic infections, and tumors which are otherwise rare in people who have normal immune function. These late symptoms of infection are referred to as acquired immunodeficiency syndrome (AIDS). This stage is often also associated with unintended weight loss.
Long-term nonprogressors (LTNPs), sometimes also called elite controllers, are individuals infected with HIV, who maintain a CD4 count greater than 500 without antiretroviral therapy with a detectable viral load. Many of these patients have been HIV positive for 30 years without progressing to the point of needing to take medication in order not to develop AIDS. They have been the subject of a great deal of research, since an understanding of their ability to control HIV infection may lead to the development of immune therapies or a therapeutic vaccine. The classification "Long-term non-progressor" is not permanent, because some patients in this category have gone on to develop AIDS.
A neutralizing antibody (NAb) is an antibody that defends a cell from a pathogen or infectious particle by neutralizing any effect it has biologically. Neutralization renders the particle no longer infectious or pathogenic. Neutralizing antibodies are part of the humoral response of the adaptive immune system against viruses, intracellular bacteria and microbial toxin. By binding specifically to surface structures (antigen) on an infectious particle, neutralizing antibodies prevent the particle from interacting with its host cells it might infect and destroy. Immunity due to neutralizing antibodies is also known as sterilizing immunity, as the immune system eliminates the infectious particle before any infection takes place.

Janice Ellen Clements is Vice Dean for Faculty at the Johns Hopkins School of Medicine and the Mary Wallace Stanton Professor of Faculty Affairs. She is a professor in the departments of Molecular and Comparative Pathobiology, Neurology, and Pathology, and has a joint appointment in molecular biology and genetics. Her molecular biology and virology research examines lentiviruses and how they cause neurological diseases.
M. Christine "Chris" Zink is the director of the Department of Molecular and Comparative Pathobiology at the Johns Hopkins School of Medicine. She also holds professorships in the Department of Pathology at Johns Hopkins and in the Department of Molecular Microbiology and Immunology at the Johns Hopkins Bloomberg School of Public Health. Zink researches the response of the immune system to retroviruses such as HIV and is currently investigating an animal model of antiretroviral therapy and the potential of a common antibiotic to prevent HIV-associated neurocognitive disorders.
Robert F. Siliciano is a professor of medicine at the Johns Hopkins University School of Medicine and an investigator with the Howard Hughes Medical Institute. Siliciano (sill-ih-CAH-noh) has a joint appointment in the Department of Molecular Biology and Genetics at Johns Hopkins. Siliciano researches the mechanisms by which the human immunodeficiency virus (HIV) remains latent in the human body.
AntiViral-HyperActivation Limiting Therapeutics (AV-HALTs) are an investigational class of antiretroviral drugs used to treat Human Immunodeficiency Virus (HIV) infection. Unlike other antiretroviral agents given to reduce viral replication, AV-HALTs are single or combination drugs designed to reduce the rate of viral replication while, at the same time, also directly reducing the state of immune system hyperactivation now believed to drive the loss of CD4+ T helper cells leading to disease progression and Acquired Immunodeficiency Syndrome (AIDS).
Stuart C. Ray is an American physician. He is Vice Chair of Medicine for Data Integrity and Analytics, Associate Director of the Infectious Diseases Fellowship Training Program at the Johns Hopkins School of Medicine, and a Professor in the Department of Medicine, Division of Infectious Diseases. Ray also holds appointments in Viral Oncology and the Division of Health Sciences Informatics. He is affiliated with the Institute for Computational Medicine at Johns Hopkins and is licensed to practice medicine in Maryland.

The stages of HIV infection are acute infection, latency and AIDS. Acute infection lasts for several weeks and may include symptoms such as fever, swollen lymph nodes, inflammation of the throat, rash, muscle pain, malaise, and mouth and esophageal sores. The latency stage involves few or no symptoms and can last anywhere from two weeks to twenty years or more, depending on the individual. AIDS, the final stage of HIV infection, is defined by low CD4+ T cell counts, various opportunistic infections, cancers and other conditions.
The co-epidemic of tuberculosis (TB) and human immunodeficiency virus (HIV) is one of the major global health challenges in the present time. The World Health Organization (WHO) reports 9.2 million new cases of TB in 2006 of whom 7.7% were HIV-infected. Tuberculosis is the most common contagious infection in HIV-Immunocompromised patients leading to death. These diseases act in combination as HIV drives a decline in immunity while tuberculosis progresses due to defective immune status. This condition becomes more severe in case of multi-drug (MDRTB) and extensively drug resistant TB (XDRTB), which are difficult to treat and contribute to increased mortality. Tuberculosis can occur at any stage of HIV infection. The risk and severity of tuberculosis increases soon after infection with HIV. A study on gold miners of South Africa revealed that the risk of TB was doubled during the first year after HIV seroconversion. Although tuberculosis can be a relatively early manifestation of HIV infection, it is important to note that the risk of tuberculosis progresses as the CD4 cell count decreases along with the progression of HIV infection. The risk of TB generally remains high in HIV-infected patients, remaining above the background risk of the general population even with effective immune reconstitution and high CD4 cell counts with antiretroviral therapy.
Deborah Persaud is a Guyanese-born American virologist who primarily works on HIV/AIDS at Johns Hopkins Children's Center.

Lauren V. Wood is an American allergist, immunologist, and staff physician at the National Cancer Institute (NCI) at the National Institutes of Health (NIH) in Bethesda, Maryland, where she has served as a principal investigator. She is known for conducting studies of vaccines for cancer, Human papillomavirus (HPV), Hepatitis C, and HIV especially for use with children, teens and young adults. She holds the rank of captain in the U.S. Public Health Service (PHS).

Sharon Ruth Lewin, FRACP, FAHMS is an Australian Infectious Disease physician and researcher, and the inaugural director of The Peter Doherty Institute for Infection and Immunity, a joint venture between the University of Melbourne and the Royal Melbourne Hospital. She leads a multi-disciplinary research team working on mechanisms of HIV latency, clinical trials advancing potential HIV cure strategies and how HIV is affected by co-infections such as Hepatitis B. Lewin has extensive experience in scientific leadership, and is a strong advocate for community engagement and partnership in research.
Ya-Chi Ho is a Taiwanese infectious disease researcher and Assistant Professor of Assistant Professor of Microbial Pathogenesis and Medicine at Yale University. Her research centers on the interaction between HIV and the host's immune system with the ultimate goal of curing HIV/AIDS.
References
- ↑ Johns Hopkins Department of Medicine, Division of Infectious Diseases faculty members
- 1 2 Infectious Diseases Society of America IDSA guide to infectious diseases training programs.
- 1 2 "'Elite' HIV wife may hold secret to AIDS vaccine" Maggie Fox, Reuters, August 12, 2008.
- ↑ "HealthGrades report: Dr. Joel N. Blankson, MD". Archived from the original on 2008-06-21. Retrieved 2009-12-31.
- 1 2 "Physician Information - Joel Blankson, MD". Archived from the original on 2011-07-10. Retrieved 2009-12-31.
- ↑ Rockefeller University News, June 16, 1996
- ↑ Blankson, J.; Loh, D.; Morse, S. (1995). "Superantigens and conventional antigens induce different responses in alpha beta T-cell receptor transgenic mice". Immunology. 85 (1): 57–62. PMC 1384024 . PMID 7635522.
- ↑ Blankson, J.; Morse, S. (1994). "The CD28/B7 pathway costimulates the response of primary murine T cells to superantigens as well as to conventional antigens". Cellular Immunology. 157 (1): 306–312. doi:10.1006/cimm.1994.1225. PMID 7518754.
- ↑ Mankowski JL, Queen SE, Fernandez CS, Tarwater PM, Karper JM, Adams RJ, Kent SJ (2008). "Natural host genetic resistance to lentiviral CNS disease: a neuroprotective MHC class I allele in SIV-infected macaques". PLOS ONE. 3 (11): e3603. Bibcode:2008PLoSO...3.3603M. doi: 10.1371/journal.pone.0003603 . PMC 2574413 . PMID 18978944.
- ↑ Blankson, J.; Finzi, D.; Pierson, T.; Sabundayo, B.; Chadwick, K.; Margolick, J.; Quinn, T.; Siliciano, R. (2000). "Biphasic decay of latently infected CD4+ T cells in acute human immunodeficiency virus type 1 infection". The Journal of Infectious Diseases. 182 (6): 1636–1642. doi: 10.1086/317615 . PMID 11069234.
- ↑ Blankson, J.; Gallant, J.; Siliciano, R. (2001). "Proliferative responses to human immunodeficiency virus type 1 (HIV-1) antigens in HIV-1-infected patients with immune reconstitution". The Journal of Infectious Diseases. 183 (4): 657–661. doi: 10.1086/318545 . PMID 11170994.
- ↑ Blankson, J. N.; Siliciano, R. F. (2001). "MHC class II genotype and the control of viremia in HIV-1–infected individuals on highly active antiretroviral therapy". Journal of Clinical Investigation. 107 (5): 549–51. doi:10.1172/JCI12430. PMC 199437 . PMID 11238554.
- ↑ Blankson, J. N.; Persaud, D.; Siliciano, R. F. (2002). "The Challenge of Viral Reservoirs in Hiv-1 Infection". Annual Review of Medicine. 53: 557–593. doi:10.1146/annurev.med.53.082901.104024. PMID 11818490.
- ↑ Blankson, J. N.; Siliciano, R. F. (2001). "Structured therapeutic interruptions: a review". The Hopkins HIV Report. 13 (1): 1, 8–9, 13. PMID 12184252.
- ↑ O’connell, K. A.; Bailey, J. R.; Blankson, J. N. (2009). "Elucidating the elite: mechanisms of control in HIV-1 infection". Trends in Pharmacological Sciences. 30 (12): 631–637. doi:10.1016/j.tips.2009.09.005. PMID 19837464.
- ↑ Blankson, J. N. (2009). "Effector mechanisms in HIV-1 infected elite controllers: Highly active immune responses?". Antiviral Research. 85 (1): 295–302. doi:10.1016/j.antiviral.2009.08.007. PMC 2814919 . PMID 19733595.
- ↑ PubMed search for Blankson JN
- ↑ "Why Some Infected With HIV Remain Symptom Free Without Antiretroviral Drugs" Science Daily, August 13, 2008.
- ↑ "Rare Case Suggests Immune Control of HIV Possible" Michael Smith, MedPage Today, August 12, 2008.
- ↑ "News in brief - Sept. 1, 2008" "Study examines HIV resistance," American Medical News, September 1, 2008.
- ↑ Aerzte Zeitung (Doctors' News) (in German) "Zehn Jahre HIV infiziert - trotzdem fast kerngesund" ("Ten years with HIV - yet almost completely healthy"), August 15, 2008.
- ↑ Globo.com (in Portuguese) "Algumas pessoas têm defesa natural contra aids, revela estudo," Globo, August 14, 2008.
- ↑ WProst24 (in Polish) "Istnieją ludzie odporni na HIV," August 14, 2008.
- ↑ Vanguardia.com (in Spanish) "Algunas personas poseen defensa natural contra Sida" ("Some people have natural defenses against AIDS"), Vanguardia (Colombia), August 16, 2008.
- ↑ italiainformazioni.com (in Italian) "Forse c'è una speranza per debellare l'Aids. I medici "studiano" il caso di una donna affetta da 10 anni senza sintomi" ("Possible hope in the fight against AIDS. Doctors study the case of a woman infected for ten years without symptoms"), Italia Informazioni, August 13, 2008.