Interleukins (ILs) are a group of cytokines that are expressed and secreted by white blood cells (leukocytes) as well as some other body cells. The human genome encodes more than 50 interleukins and related proteins.

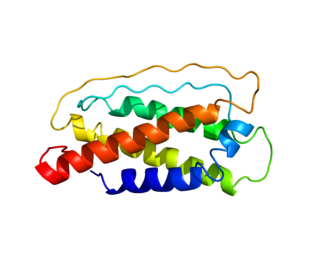
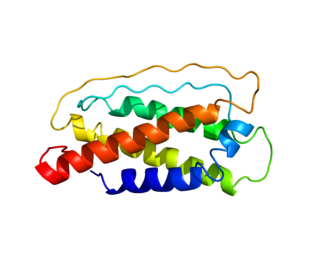
Interleukin 10 (IL-10), also known as human cytokine synthesis inhibitory factor (CSIF), is an anti-inflammatory cytokine. In humans, interleukin 10 is encoded by the IL10 gene. IL-10 signals through a receptor complex consisting of two IL-10 receptor-1 and two IL-10 receptor-2 proteins. Consequently, the functional receptor consists of four IL-10 receptor molecules. IL-10 binding induces STAT3 signalling via the phosphorylation of the cytoplasmic tails of IL-10 receptor 1 + IL-10 receptor 2 by JAK1 and Tyk2 respectively.
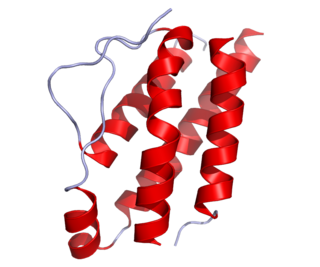
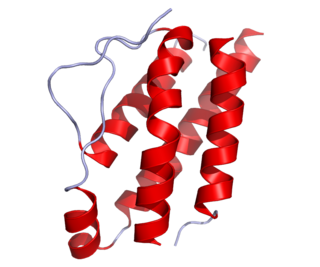
Interleukin-2 (IL-2) is an interleukin, a type of cytokine signaling molecule in the immune system. It is a 15.5–16 kDa protein that regulates the activities of white blood cells (leukocytes, often lymphocytes) that are responsible for immunity. IL-2 is part of the body's natural response to microbial infection, and in discriminating between foreign ("non-self") and "self". IL-2 mediates its effects by binding to IL-2 receptors, which are expressed by lymphocytes. The major sources of IL-2 are activated CD4+ T cells and activated CD8+ T cells. Put shortly the function of IL-2 is to stimulate the growth of helper, cytotoxic and regulatory T cells.

The interleukin 4 is a cytokine that induces differentiation of naive helper T cells (Th0 cells) to Th2 cells. Upon activation by IL-4, Th2 cells subsequently produce additional IL-4 in a positive feedback loop. IL-4 is produced primarily by mast cells, Th2 cells, eosinophils and basophils. It is closely related and has functions similar to IL-13.

The common gamma chain (γc), also known as interleukin-2 receptor subunit gamma or IL-2RG, is a cytokine receptor sub-unit that is common to the receptor complexes for at least six different interleukin receptors: IL-2, IL-4, IL-7, IL-9, IL-15 and interleukin-21 receptor. The γc glycoprotein is a member of the type I cytokine receptor family expressed on most lymphocyte populations, and its gene is found on the X-chromosome of mammals.
Interleukin 7 (IL-7) is a protein that in humans is encoded by the IL7 gene.

CD28 is a protein expressed on T cells that provides essential co-stimulatory signals required for T cell activation and survival. When T cells are stimulated through CD28 in conjunction with the T-cell receptor (TCR), it enhances the production of various interleukins, particularly IL-6. CD28 serves as a receptor for CD80 (B7.1) and CD86 (B7.2), proteins found on antigen-presenting cells (APCs).

Interleukin-1 beta (IL-1β) also known as leukocytic pyrogen, leukocytic endogenous mediator, mononuclear cell factor, lymphocyte activating factor and other names, is a cytokine protein that in humans is encoded by the IL1B gene. There are two genes for interleukin-1 (IL-1): IL-1 alpha and IL-1 beta. IL-1β precursor is cleaved by cytosolic caspase 1 to form mature IL-1β.

Interleukin 21 (IL-21) is a protein that in humans is encoded by the IL21 gene.

Interleukin-22 (IL-22) is a protein that in humans is encoded by the IL22 gene.

The interleukin 4 receptor is a type I cytokine receptor. It is a heterodimer, that is, composed of two subunits. IL4R is the human gene coding for IL-4Rα, the subunit which combines with either common gamma chain or with IL-13Rα1.

Subunit beta of interleukin 12 is a protein subunit that in humans is encoded by the IL12B gene. IL-12B is a common subunit of interleukin 12 and interleukin 23.

Interleukin 6 receptor (IL6R) also known as CD126 is a type I cytokine receptor.

Interleukin-12 subunit alpha is a protein that in humans is encoded by the IL12A gene.

Interleukin 10 receptor, beta subunit is a subunit for the interleukin-10 receptor. IL10RB is its human gene.

Interleukin 21 receptor is a type I cytokine receptor. IL21R is its human gene.

The interleukin-2 receptor alpha chain is a protein involved in the assembly of the high-affinity interleukin-2 receptor, consisting of alpha (IL2RA), beta (IL2RB) and the common gamma chain (IL2RG). As the name indicates, this receptor interacts with interleukin-2, a pleiotropic cytokine which plays an important role in immune homeostasis.
The NSG mouse is a brand of immunodeficient laboratory mice, developed and marketed by Jackson Laboratory, which carries the strain NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ. NSG branded mice are among the most immunodeficient described to date. NSG branded mice lack mature T cells, B cells, and natural killer (NK) cells. NSG branded mice are also deficient in multiple cytokine signaling pathways, and they have many defects in innate immunity. The compound immunodeficiencies in NSG branded mice permit the engraftment of a wide range of primary human cells, and enable sophisticated modeling of many areas of human biology and disease. NSG branded mice were developed in the laboratory of Dr. Leonard Shultz at Jackson Laboratory, which owns the NSG trade mark.
Paola Ricciardi-Castagnoli is an Italian immunologist based in Siena. Paola is the scientific director of Toscana Life Sciences Foundation (TLS) in Siena. She was former scientific director of the Singapore Immunology Network (SIgN).
Gene Martin Shearer is an American immunologist who works at the National Institutes of Health (NIH). He first achieved fame for his discovery in 1974 that T lymphocytes recognized chemically modified surface antigens only in the context of self major histocompatibility complex (MHC) encoded molecules, identifying the central feature of antigen recognition by T lymphocytes known as MHC restriction. His discovery of MHC restriction using chemically modified surface antigens was simultaneous with the discovery of MHC restricted T lymphocyte recognition of virus infected cells by Rolf Zinkernagel and Peter Doherty, who received the 1996 Nobel Prize in Physiology or Medicine.