Neurosurgery or neurological surgery, known in common parlance as brain surgery, is the medical specialty concerned with the surgical treatment of disorders which affect any portion of the nervous system including the brain, spinal cord and peripheral nervous system.

Lumbar spinal stenosis (LSS) is a medical condition in which the spinal canal narrows and compresses the nerves and blood vessels at the level of the lumbar vertebrae. Spinal stenosis may also affect the cervical or thoracic region, in which case it is known as cervical spinal stenosis or thoracic spinal stenosis. Lumbar spinal stenosis can cause pain in the low back or buttocks, abnormal sensations, and the absence of sensation (numbness) in the legs, thighs, feet, or buttocks, or loss of bladder and bowel control.

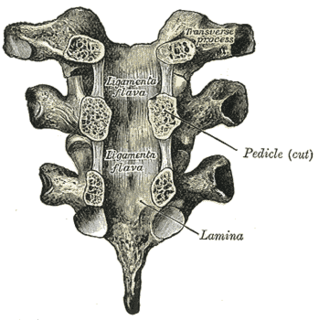
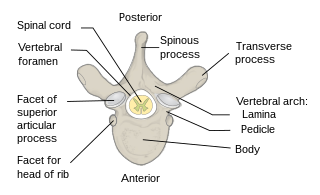
A laminectomy is a surgical procedure that removes a portion of a vertebra called the lamina, which is the roof of the spinal canal. It is a major spine operation with residual scar tissue and may result in postlaminectomy syndrome. Depending on the problem, more conservative treatments may be viable.

Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related wear and tear of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.
Myelopathy describes any neurologic deficit related to the spinal cord. When due to trauma, it is known as (acute) spinal cord injury. When inflammatory, it is known as myelitis. Disease that is vascular in nature is known as vascular myelopathy. The most common form of myelopathy in humans, cervical spondylotic myelopathy (CSM), is caused by arthritic changes (spondylosis) of the cervical spine, which result in narrowing of the spinal canal ultimately causing compression of the spinal cord. In Asian populations, spinal cord compression often occurs due to a different, inflammatory process affecting the posterior longitudinal ligament.

Degenerative disc disease (DDD) is a medical condition typically brought on by the normal aging process in which there are anatomic changes and possibly a loss of function of one or more intervertebral discs of the spine. DDD can take place with or without symptoms, but is typically identified once symptoms arise. The root cause is thought to be loss of soluble proteins within the fluid contained in the disc with resultant reduction of the oncotic pressure, which in turn causes loss of fluid volume. Normal downward forces cause the affected disc to lose height, and the distance between vertebrae is reduced. The anulus fibrosus, the tough outer layers of a disc, also weakens. This loss of height causes laxity of the longitudinal ligaments, which may allow anterior, posterior, or lateral shifting of the vertebral bodies, causing facet joint malalignment and arthritis; scoliosis; cervical hyperlordosis; thoracic hyperkyphosis; lumbar hyperlordosis; narrowing of the space available for the spinal tract within the vertebra ; or narrowing of the space through which a spinal nerve exits with resultant inflammation and impingement of a spinal nerve, causing a radiculopathy.

Spinal fusion, also called spondylodesis or spondylosyndesis, is a neurosurgical or orthopedic surgical technique that joins two or more vertebrae. This procedure can be performed at any level in the spine and prevents any movement between the fused vertebrae. There are many types of spinal fusion and each technique involves using bone grafting—either from the patient (autograft), donor (allograft), or artificial bone substitutes—to help the bones heal together. Additional hardware is often used to hold the bones in place while the graft fuses the two vertebrae together. The placement of hardware can be guided by fluoroscopy, navigation systems, or robotics.
Wobbler disease is a catchall term referring to several possible malformations of the cervical vertebrae that cause an unsteady (wobbly) gait and weakness in dogs and horses. A number of different conditions of the cervical (neck) spinal column cause similar clinical signs. These conditions may include malformation of the vertebrae, intervertebral disc protrusion, and disease of the interspinal ligaments, ligamenta flava, and articular facets of the vertebrae. Wobbler disease is also known as cervical vertebral instability, cervical spondylomyelopathy (CSM), and cervical vertebral malformation (CVM). In dogs, the disease is most common in large breeds, especially Great Danes and Doberman Pinschers. In horses, it is not linked to a particular breed, though it is most often seen in tall, race-bred horses of Thoroughbred or Standardbred ancestry. It is most likely inherited to at least some extent in dogs and horses.
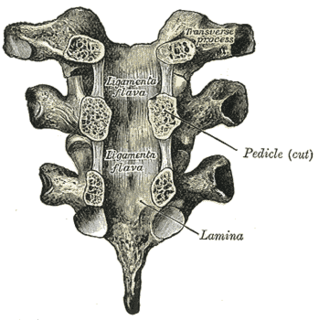
The ligamenta flava are a series of ligaments that connect the ventral parts of the laminae of adjacent vertebrae. They help to preserve upright posture, preventing hyperflexion, and ensuring that the vertebral column straightens after flexion. Hypertrophy can cause spinal stenosis.
Microsurgical lumbar laminoplasty is a minimally invasive technique for decompressing pinched nerves in the lumbar spine. Pinched or compressed nerves may result from herniated discs, lumbar spinal stenosis, or spondylolisthesis.

Spinal disc herniation is an injury to the cushioning and connective tissue between vertebrae, usually caused by excessive strain or trauma to the spine. It may result in back pain, pain or sensation in different parts of the body, and physical disability. The most conclusive diagnostic tool for disc herniation is MRI, and treatment may range from painkillers to surgery. Protection from disc herniation is best provided by core strength and an awareness of body mechanics including posture.

Anterior cervical discectomy and fusion (ACDF) is a surgical procedure to treat nerve root or spinal cord compression by decompressing the spinal cord and nerve roots of the cervical spine with a discectomy, followed by inter-vertebral fusion to stabilize the corresponding vertebrae. This procedure is used when other non-surgical treatments have failed.

Cervical spinal stenosis is a bone disease involving the narrowing of the spinal canal at the level of the neck. It is frequently due to chronic degeneration, but may also be congenital. Treatment is frequently surgical.

Neurogenic claudication (NC), also known as pseudoclaudication, is the most common symptom of lumbar spinal stenosis (LSS) and describes intermittent leg pain from impingement of the nerves emanating from the spinal cord. Neurogenic means that the problem originates within the nervous system. Claudication, from the Latin word for to limp, refers to painful cramping or weakness in the legs. NC should therefore be distinguished from vascular claudication, which stems from a circulatory problem rather than a neural one.

A laminotomy is an orthopaedic neurosurgical procedure that removes part of the lamina of a vertebral arch in order to relieve pressure in the vertebral canal. A laminotomy is less invasive than conventional vertebral column surgery techniques, such as laminectomy because it leaves more ligaments and muscles attached to the vertebral column intact and it requires removing less bone from the vertebra. As a result, laminotomies typically have a faster recovery time and result in fewer postoperative complications. Nevertheless, possible risks can occur during or after the procedure like infection, hematomas, and dural tears. Laminotomies are commonly performed as treatment for lumbar spinal stenosis and herniated disks. MRI and CT scans are often used pre- and post surgery to determine if the procedure was successful.

Spinal decompression is the relief of pressure on the spinal cord or on one or more compressed nerve roots passing through or exiting the spinal column. Decompression of the spinal neural elements is a key component in treating spinal radiculopathy, myelopathy and claudication.

Spinal stenosis is an abnormal narrowing of the spinal canal or neural foramen that results in pressure on the spinal cord or nerve roots. Symptoms may include pain, numbness, or weakness in the arms or legs. Symptoms are typically gradual in onset and improve with bending forwards. Severe symptoms may include loss of bladder control, loss of bowel control, or sexual dysfunction.
The ventral slot technique is a procedure that allows the surgeon to reach and decompress the spinal cord and associated nerve roots from a ventral route in veterinary medicine. There are also alternative ways to open the spinal canal from dorsal by performing a hemilaminectomy, but this often gives only limited access. Even when the main pathological changes evolve from the midline, it is necessary to choose a ventral approach.
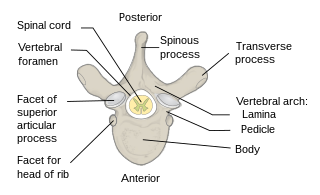
The spinal column, characteristic of each vertebrate species, is a moderately flexible series of vertebrae, each constituting a characteristic irregular bone whose complex structure is composed primarily of bone, and secondarily of hyaline cartilage. They show variation in the proportion contributed by these two tissue types; such variations correlate on one hand with the cerebral/caudal rank, and on the other with phylogenetic differences among the vertebrate taxa.

Ossification of the posterior longitudinal ligament (OPLL) is a process of fibrosis, calcification, and ossification of the posterior longitudinal ligament of the spine, that may involve the spinal dura. Once considered a disorder unique to people of Asian heritage, it is now recognized as an uncommon disorder in a variety of patients with myelopathy.