Prostate cancer is cancer of the prostate. The prostate is a gland in the male reproductive system that surrounds the urethra just below the bladder. Most prostate cancers are slow growing. Cancerous cells may spread to other areas of the body, particularly the bones and lymph nodes. It may initially cause no symptoms. In later stages, symptoms include pain or difficulty urinating, blood in the urine, or pain in the pelvis or back. Benign prostatic hyperplasia may produce similar symptoms. Other late symptoms include fatigue, due to low levels of red blood cells.

Bladder cancer is any of several types of cancer arising from the tissues of the urinary bladder. Symptoms include blood in the urine, pain with urination, and low back pain. It is caused when epithelial cells that line the bladder become malignant.

Lumpectomy is a surgical removal of a discrete portion or "lump" of breast tissue, usually in the treatment of a malignant tumor or breast cancer. It is considered a viable breast conservation therapy, as the amount of tissue removed is limited compared to a full-breast mastectomy, and thus may have physical and emotional advantages over more disfiguring treatment. Sometimes a lumpectomy may be used to either confirm or rule out that cancer has actually been detected. A lumpectomy is usually recommended to patients whose cancer has been detected early and who do not have enlarged tumors. Although a lumpectomy is used to allow for most of the breast to remain intact, the procedure may result in adverse affects that can include sensitivity and result in scar tissue, pain, and possible disfiguration of the breast if the lump taken out is significant. According to National Comprehensive Cancer Network guidelines, lumpectomy may be performed for ductal carcinoma in situ (DCIS), invasive ductal carcinoma, or other conditions.

Cystectomy is a medical term for surgical removal of all or part of the urinary bladder. It may also be rarely used to refer to the removal of a cyst. The most common condition warranting removal of the urinary bladder is bladder cancer.

Prostatectomy as a medical term refers to the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.
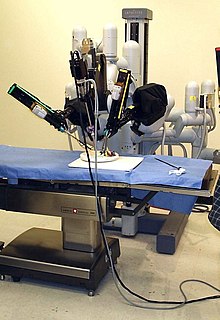
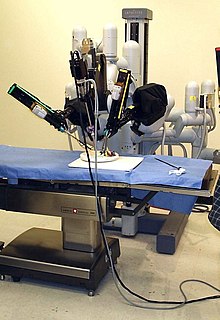
Robotic surgery are types of surgical procedures that are done using robotic systems. Robotically-assisted surgery was developed to try to overcome the limitations of pre-existing minimally-invasive surgical procedures and to enhance the capabilities of surgeons performing open surgery.

The sentinel lymph node is the hypothetical first lymph node or group of nodes draining a cancer. In case of established cancerous dissemination it is postulated that the sentinel lymph node/s is/are the target organs primarily reached by metastasizing cancer cells from the tumor.

Radical retropubic prostatectomy is a surgical procedure in which the prostate gland is removed through an incision in the abdomen. It is most often used to treat individuals who have early prostate cancer. Radical retropubic prostatectomy can be performed under general, spinal, or epidural anesthesia and requires blood transfusion less than one-fifth of the time. Radical retropubic prostatectomy is associated with complications such as urinary incontinence and impotence, but these outcomes are related to a combination of individual patient anatomy, surgical technique, and the experience and skill of the surgeon.

Radical perineal prostatectomy is a surgical procedure wherein the entire prostate gland is removed through an incision in the area between the anus and the scrotum (perineum).
Total mesorectal excision (TME) is a standard surgical technique for treatment of rectal cancer, first described in 1982 by Professor Bill Heald at the UK's Basingstoke District Hospital. It is a precise dissection of the mesorectal envelope comprising rectum containing the tumour together with all the surrounding fatty tissue and the sheet of tissue that contains lymph nodes and blood vessels. Dissection is along the avascular alveolar plane between the presacral and mesorectal fascia, described as holy plane. Dissection along this plane facilitates a straightforward dissection and preserves the sacral vessels and hypogastric nerves and is a sphincter-sparing resection and decreases permanent stoma rates. It is possible to rejoin the two ends of the colon; however, most patients require a temporary ileostomy pouch to bypass the colon, allowing it to heal with less risk of infection, perforation or leakage.

Breast-conserving surgery (BCS) refers to an operation that aims to remove breast cancer while avoiding a mastectomy. Other terms for this operation include: lumpectomy, wide local excision, segmental resection, tylectomy, and quadrantectomy. BCS has been increasingly accepted as an alternative to mastectomy in specific patients, as it provides tumor removal while maintaining an acceptable cosmetic outcome. This page reviews the history of this operation, important considerations in decision making and patient selection, and the emerging field of oncoplastic breast conservation surgery.

Brachytherapy is a type of radiotherapy, or radiation treatment, offered to certain cancer patients. There are two types of brachytherapy – high dose-rate (HDR) and low dose-rate (LDR). LDR brachytherapy is the one most commonly used to treat prostate cancer. It may be referred to as 'seed implantation' or it may be called 'pinhole surgery'.

Mani Menon, born 9 July 1948 in Trichur, India, is an American surgeon whose pioneering work has helped to lay the foundation for modern robotic cancer surgery. He is the founding director and the Raj and Padma Vattikuti Distinguished Chair of the Vattikuti Urology Institute at the Henry Ford Hospital in Detroit, MI, where he established the first cancer-oriented robotics program in the world. Menon is widely regarded for his role in the development of robotic surgery techniques for the treatment of patients with prostate, kidney, and bladder cancers, as well as for the development of robotic kidney transplantation.
Menon is the recipient of the Gold Cystoscope award, Hugh Hampton Young award, the Keyes Medal, the prestigious B.C. Roy award.

Ashutosh K. Tewari is the chairman of urology at the Icahn School of Medicine at Mount Sinai Hospital in New York City. He is a board certified American urologist, oncologist, and principal investigator. Before moving to the Icahn School of Medicine in 2013, he was the founding director of both the Center for Prostate Cancer at Weill Cornell Medical College and the LeFrak Center for Robotic Surgery at NewYork–Presbyterian Hospital. Dr. Tewari was the Ronald P. Lynch endowed Chair of Urologic Oncology and the hospital's Director of Robotic Prostatectomy, treating patients with prostate, urinary bladder and other urological cancers. He is the current President of the Society for Urologic Robotic Surgeons (SURS) and the Committee Chair of the Prostate Program. Dr. Tewari is a world leading urological surgeon, and has performed over 9,000 robotically assisted procedures using the da Vinci Surgical System. Academically, he is recognized as a world-renowned expert on urologic oncology with over 250 peer reviewed published papers to his credit; he is on such lists as America's Top Doctors, New York Magazine's Best Doctors, and Who's Who in the World. In 2012, he was given the American Urological Association Gold Cystoscope Award for "outstanding contributions to the field of urologic oncology, most notably the treatment of prostate cancer and the development of novel techniques to improve the outcomes of robotic prostatectomy."
Treatment for prostate cancer may involve active surveillance, surgery, radiation therapy – including brachytherapy and external-beam radiation therapy, proton therapy, high-intensity focused ultrasound (HIFU), cryosurgery, hormonal therapy, chemotherapy, or some combination. Treatments also extend to survivorship based interventions. These interventions are focused on five domains including: physical symptoms, psychological symptoms, surveillance, health promotion and care coordination. However, a published review has found only high levels of evidence for interventions that target physical and psychological symptom management and health promotion, with no reviews of interventions for either care coordination or surveillance. The favored treatment option depends on the stage of the disease, the Gleason score, and the PSA level. Other important factors include the man's age, his general health, and his feelings about potential treatments and their possible side-effects. Because all treatments can have significant side-effects, such as erectile dysfunction and urinary incontinence, treatment discussions often focus on balancing the goals of therapy with the risks of lifestyle alterations.

Dr. Michael A. Palese, is an American urologist specializing in robotic, laparoscopic and endoscopic surgery, with a special emphasis on robotic surgeries relating to kidney cancer and kidney stone disease.

Roger Sinclair Kirby FRCS(Urol), FEBU is a British retired prostate surgeon and professor of urology, researcher, writer on men's health and prostate disease, founding editor of the journal Prostate Cancer and Prostatic Diseases and Trends in Urology and Men's Health and a fundraiser for prostate disease charities, best known for his use of the da Vinci surgical robot for laparoscopic prostatectomy in the treatment of prostate cancer. He is a co-founder and president of the charity The Urology Foundation (TUF), vice-president of the charity Prostate Cancer UK, trustee of the King Edward VII's Hospital and as of 2020 is president of the Royal Society of Medicine (RSM), London.
Mark S. Soloway is a leading authority in urologic cancer, researcher, former departmental Chair, medical professor and invitational lecturer. He served as Chairman of the University of Miami Miller School of Medicine Department of Urology and is currently a Professor at the Miller School of Medicine. Born in Cleveland, Soloway received his B.S. from Northwestern University in Chicago, Il (1961–1964) and completed his M.D. and residency at Case Western Reserve University School of Medicine in Cleveland, Ohio (1964–1970). He completed a fellowship at the National Cancer Institute of the National Institute of Health in Bethesda, MD (1970–1972). Soloway has received numerous awards for his work as a researcher and teacher, including the American Urological Association's Gold Cystoscope Award “For the individual who has contributed most to the field of urology within ten years of completion of his residency program” (1984), Mosby Scholarship for Scholastic Excellence (1967), North Central Section of American Urological Association Traveling Fellowship Award (1972) and many others.

Michael D. Stifelman, M.D.,, an internationally recognized American physician and urologist, is known for his work in upper tract urinary reconstructive surgery and use of multi- and single-port robotic surgical technology to perform complex cancer and non-cancer urological procedures. An innovator in the field of urological surgery, Dr. Stifelman leads a renowned Center of Excellence for robotic surgery at Hackensack University Medical Center in Hackensack, New Jersey, and serves as chair of the hospital’s Department of Urology.

Vipul R. Patel, FACS is the founder and Medical Director of the Florida Hospital Global Robotics Institute, founder and Vice President of the Society of Robotic Surgery, and founder and Editor Emeritus of The Journal of Robotic Surgery. He is board certified by the American Urological Association and specializes in robotic surgery for prostate cancer. As of February, 2018 he performed his 11,000th robotic-assisted prostatectomy. The large volume of prostatectomies he has performed has enabled him to amass a large amount of statistical evidence regarding the efficacy of robotic techniques which has been used in developing and refining techniques. Patel credits the use of robotic assisted surgery with helping surgeons achieve better surgical outcomes with the "trifecta" of cancer control, continence and sexual function. In the course of his career Patel has led and participated in studies that have resulted in developing improved outcomes for robotic surgery and urologic treatment.