Osteoporosis is a systemic skeletal disorder characterized by low bone mass, micro-architectural deterioration of bone tissue leading to bone fragility, and consequent increase in fracture risk. It is the most common reason for a broken bone among the elderly. Bones that commonly break include the vertebrae in the spine, the bones of the forearm, and the hip. Until a broken bone occurs there are typically no symptoms. Bones may weaken to such a degree that a break may occur with minor stress or spontaneously. After the broken bone heals, the person may have chronic pain and a decreased ability to carry out normal activities.

Compartment syndrome is a condition in which increased pressure within one of the body's anatomical compartments results in insufficient blood supply to tissue within that space. There are two main types: acute and chronic. Compartments of the leg or arm are most commonly involved.
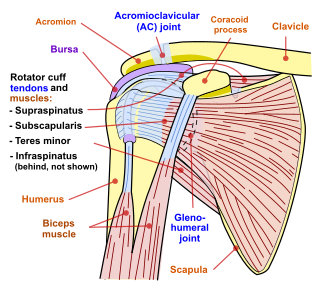
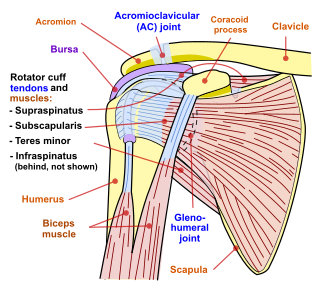
Shoulder problems including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well.

Fibromyalgia (FM) is a medical condition defined by the presence of chronic widespread pain, fatigue, waking unrefreshed, cognitive symptoms, lower abdominal pain or cramps, and depression. Other symptoms include insomnia and a general hypersensitivity.

Piriformis syndrome is a condition which is believed to result from compression of the sciatic nerve by the piriformis muscle. Symptoms may include pain and numbness in the buttocks and down the leg. Often symptoms are worsened with sitting or running.

A stress fracture is a fatigue-induced bone fracture caused by repeated stress over time. Instead of resulting from a single severe impact, stress fractures are the result of accumulated injury from repeated submaximal loading, such as running or jumping. Because of this mechanism, stress fractures are common overuse injuries in athletes.
Manual therapy, or manipulative therapy, is a physical treatment primarily used by physical therapists, physiotherapists, occupational therapists to treat musculoskeletal pain and disability; it mostly includes kneading and manipulation of muscles, joint mobilization and joint manipulation. It is also used by Rolfers, massage therapists, athletic trainers, osteopaths, and physicians.

A rotator cuff tear is an injury where one or more of the tendons or muscles of the rotator cuff of the shoulder get torn. Symptoms may include shoulder pain, which is often worse with movement, or weakness. This may limit people's ability to brush their hair or put on clothing. Clicking may also occur with movement of the arm.

A shin splint, also known as medial tibial stress syndrome, is pain along the inside edge of the shinbone (tibia) due to inflammation of tissue in the area. Generally this is between the middle of the lower leg and the ankle. The pain may be dull or sharp, and is generally brought on by high-impact exercise that overloads the tibia. It generally resolves during periods of rest. Complications may include stress fractures.

Osgood–Schlatter disease (OSD) is inflammation of the patellar ligament at the tibial tuberosity (apophysitis). It is characterized by a painful bump just below the knee that is worse with activity and better with rest. Episodes of pain typically last a few weeks to months. One or both knees may be affected and flares may recur.

Osteopenia, preferably known as "low bone mass" or "low bone density", is a condition in which bone mineral density is low. Because the bones are weaker, people with osteopenia may have a higher risk of fractures, and some people may go on to develop osteoporosis. In 2010, 43 million older adults in the US had osteopenia. Unlike osteoporosis, osteopenia does not usually cause symptoms, and losing bone density in itself does not cause pain.

The psoas major is a long fusiform muscle located in the lateral lumbar region between the vertebral column and the brim of the lesser pelvis. It joins the iliacus muscle to form the iliopsoas. In animals, this muscle is equivalent to the tenderloin.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.
Orthopedic pathology, also known as bone pathology is a subspecialty of surgical pathology which deals with the diagnosis and feature of many bone diseases, specifically studying the cause and effects of disorders of the musculoskeletal system. It uses gross and microscopic findings along with the findings of in vivo radiological studies, and occasionally, specimen radiographs to diagnose diseases of the bones.
Senile osteoporosis has been recently recognized as a geriatric syndrome with a particular pathophysiology. There are different classification of osteoporosis: primary, in which bone loss is a result of aging and secondary, in which bone loss occurs from various clinical and lifestyle factors. Primary, or involuntary osteoporosis, can further be classified into Type I or Type II. Type I refers to postmenopausal osteoporosis and is caused by the deficiency of estrogen. While senile osteoporosis is categorized as an involuntary, Type II, and primary osteoporosis, which affects both men and women over the age of 70 years. It is accompanied by vitamin D deficiency, body's failure to absorb calcium, and increased parathyroid hormone.

Frailty is a common geriatric syndrome that embodies an elevated risk of catastrophic declines in health and function among older adults. Frailty is a condition associated with ageing, and it has been recognized for centuries. It is also a marker of a more widespread syndrome of frailty, with associated weakness, slowing, decreased energy, lower activity, and, when severe, unintended weight loss. Frailty has been identified as a risk factor for the development of dementia.

Patellofemoral pain syndrome is knee pain as a result of problems between the kneecap and the femur. The pain is generally in the front of the knee and comes on gradually. Pain may worsen with sitting, excessive use, or climbing and descending stairs.

Neurogenic claudication (NC), also known as pseudoclaudication, is the most common symptom of lumbar spinal stenosis (LSS) and describes intermittent leg pain from impingement of the nerves emanating from the spinal cord. Neurogenic means that the problem originates within the nervous system. Claudication, from the Latin word for to limp, refers to painful cramping or weakness in the legs. NC should therefore be distinguished from vascular claudication, which stems from a circulatory problem rather than a neural one.
Signs and symptoms of pregnancy are common, benign conditions that result from the changes to the body that occur during pregnancy. Signs and symptoms of pregnancy typically change as pregnancy progresses, although several symptoms may be present throughout. Depending on severity, common symptoms in pregnancy can develop into complications. Pregnancy symptoms may be categorized based on trimester as well as region of the body affected.

Iliocostal friction syndrome, also known as costoiliac impingement syndrome, is a condition in which the costal margin comes in contact with the iliac crest. The condition presents as low back pain which may radiate to other surrounding areas as a result of irritated nerve, tendon, and muscle structures. It may occur unilaterally due to conditions such as scoliosis, or bilaterally due to conditions such as osteoporosis and hyperkyphosis.