Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum subspecies pallidum. The signs and symptoms depend on the stage it presents: primary, secondary, latent or tertiary. The primary stage classically presents with a single chancre though there may be multiple sores. In secondary syphilis, a diffuse rash occurs, which frequently involves the palms of the hands and soles of the feet. There may also be sores in the mouth or vagina. Latent syphilis has no symptoms and can last years. In tertiary syphilis, there are gummas, neurological problems, or heart symptoms. Syphilis has been known as "the great imitator" because it may cause symptoms similar to many other diseases.

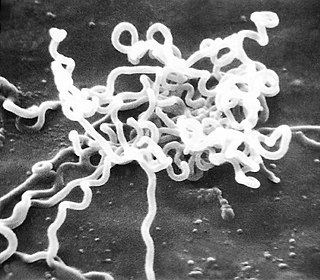
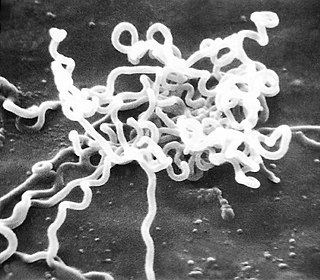
Treponema pallidum, formerly known as Spirochaeta pallida, is a microaerophilic, gram-negative, spirochaete bacterium with subspecies that cause the diseases syphilis, bejel, and yaws. It is known to be transmitted only among humans and baboons. It is a helically coiled microorganism usually 6–15 μm long and 0.1–0.2 μm wide. T. pallidum's lack of both a tricarboxylic acid cycle and processes for oxidative phosphorylation results in minimal metabolic activity. The treponemes have cytoplasmic and outer membranes. Using light microscopy, treponemes are visible only by using dark-field illumination. T. pallidum consists of three subspecies, T. p. pallidum, T. p. endemicum, and T. p. pertenue, each of which has a distinct associated disease. The ability of T. pallidum to avoid host immune defenses has allowed for stealth pathogenicity. The unique outer membrane structure and minimal expression of surface proteins of T. pallidum has made vaccine development difficult. Treponema pallidum can be treated with antibiotics such as penicillin.

Yaws is a tropical infection of the skin, bones, and joints caused by the spirochete bacterium Treponema pallidum pertenue. The disease begins with a round, hard swelling of the skin, 2 to 5 cm in diameter. The center may break open and form an ulcer. This initial skin lesion typically heals after 3–6 months. After weeks to years, joints and bones may become painful, fatigue may develop, and new skin lesions may appear. The skin of the palms of the hands and the soles of the feet may become thick and break open. The bones may become misshapen. After 5 years or more, large areas of skin may die, leaving scars.

Tabes dorsalis is a late consequence of neurosyphilis, characterized by the slow degeneration of the neural tracts primarily in the dorsal root ganglia of the spinal cord. These patients have lancinating nerve root pain which is aggravated by coughing, and features of sensory ataxia with ocular involvement.
The rapid plasma reagin test is a type of rapid diagnostic test that looks for non-specific antibodies in the blood of the patient that may indicate an infection by syphilis or related non-venereal treponematoses. It is one of several nontreponemal tests for syphilis. The term reagin means that this test does not look for antibodies against the bacterium itself, Treponema pallidum, but rather for antibodies against substances released by cells when they are damaged by T. pallidum. Traditionally, syphilis serologic testing has been performed using a nontreponemal test (NTT) such as the RPR or VDRL test, with positive results then confirmed using a specific treponemal test (TT) such as TPPA or FTA-ABS. This method is endorsed by the U.S. Centers for Disease Control and Prevention (CDC) and is the standard in many parts of the world. After screening for syphilis, a titer can be used to track the progress of the disease over time and its response to therapy.

The Venereal Disease Research Laboratory test (VDRL) is a blood test for syphilis and related non-venereal treponematoses that was developed by the eponymous US laboratory. The VDRL test is used to screen for syphilis, whereas other, more specific tests are used to diagnose the disease.

Chancroid is a bacterial sexually transmitted infection characterized by painful sores on the genitalia. Chancroid is known to spread from one individual to another solely through sexual contact. However, there have been reports of accidental infection through the hand.

Congenital syphilis is syphilis that occurs when a mother with untreated syphilis passes the infection to her baby during pregnancy or at birth. It may present in the fetus, infant, or later. Clinical features vary and differ between early onset, that is presentation before 2-years of age, and late onset, presentation after age 2-years. Infection in the unborn baby may present as poor growth, non-immune hydrops leading to premature birth or loss of the baby, or no signs. Affected newborns mostly initially have no clinical signs. They may be small and irritable. Characteristic features include a rash, fever, large liver and spleen, a runny and congested nose, and inflammation around bone or cartilage. There may be jaundice, large glands, pneumonia, meningitis, warty bumps on genitals, deafness or blindness. Untreated babies that survive the early phase may develop skeletal deformities including deformity of the nose, lower legs, forehead, collar bone, jaw, and cheek bone. There may be a perforated or high arched palate, and recurrent joint disease. Other late signs include linear perioral tears, intellectual disability, hydrocephalus, and juvenile general paresis. Seizures and cranial nerve palsies may first occur in both early and late phases. Eighth nerve palsy, interstitial keratitis and small notched teeth may appear individually or together; known as Hutchinson's triad.
Pinta is a human skin disease caused by infection with the spirochete Treponema carateum, which is morphologically and serologically indistinguishable from the bacterium that causes syphilis and bejel. The disease was previously known to be endemic to Mexico, Central America, and South America; it may have been eradicated since, with the latest case occurring in Brazil in 2020.

Aseptic meningitis is the inflammation of the meninges, a membrane covering the brain and spinal cord, in patients whose cerebral spinal fluid test result is negative with routine bacterial cultures. Aseptic meningitis is caused by viruses, mycobacteria, spirochetes, fungi, medications, and cancer malignancies. The testing for both meningitis and aseptic meningitis is mostly the same. A cerebrospinal fluid sample is taken by lumbar puncture and is tested for leukocyte levels to determine if there is an infection and goes on to further testing to see what the actual cause is. The symptoms are the same for both meningitis and aseptic meningitis but the severity of the symptoms and the treatment can depend on the certain cause.

Bejel, or endemic syphilis, is a chronic skin and tissue disease caused by infection by the endemicum subspecies of the spirochete Treponema pallidum. Bejel is one of the "endemic treponematoses", a group that also includes yaws and pinta. Typically, endemic trepanematoses begin with localized lesions on the skin or mucous membranes. Pinta is limited to affecting the skin, whereas bejel and yaws are considered to be invasive because they can also cause disease in bone and other internal tissues.

Neurosyphilis is the infection of the central nervous system in a patient with syphilis. In the era of modern antibiotics, the majority of neurosyphilis cases have been reported in HIV-infected patients. Meningitis is the most common neurological presentation in early syphilis. Tertiary syphilis symptoms are exclusively neurosyphilis, though neurosyphilis may occur at any stage of infection.
The fluorescent treponemal antibody absorption (FTA-ABS) test is a diagnostic test for syphilis. Using antibodies specific for the Treponema pallidum species, such tests would be assumed to be more specific than non-treponemal testing such as VDRL but have been shown repeatedly to be sensitive but not specific for the diagnosis of neurosyphilis in cerebrospinal fluid (CSF). In addition, FTA-ABS turns positive earlier and remains positive longer than VDRL. Other treponemes, such as T. pertenue, may also produce a positive FTA-ABS. The ABS suffix refers particularly to a processing step used to remove nonspecific antispirochetal antibodies present in normal serum.

Syphilitic aortitis is inflammation of the aorta associated with the tertiary stage of syphilis infection. SA begins as inflammation of the outermost layer of the blood vessel, including the blood vessels that supply the aorta itself with blood, the vasa vasorum. As SA worsens, the vasa vasorum undergo hyperplastic thickening of their walls thereby restricting blood flow and causing ischemia of the outer two-thirds of the aortic wall. Starved for oxygen and nutrients, elastic fibers become patchy and smooth muscle cells die. If the disease progresses, syphilitic aortitis leads to an aortic aneurysm. Overall, tertiary syphilis is a rare cause of aortic aneurysms. Syphilitic aortitis has become rare in the developed world with the advent of penicillin treatments after World War II.

A genital ulcer is an open sore located on the genital area, which includes the vulva, penis, perianal region, or anus. Genital ulcers are most commonly caused by infectious agents. However, this is not always the case, as a genital ulcer may have noninfectious causes as well.
Treponema denticola is a Gram-negative, obligate anaerobic, motile and highly proteolytic spirochete bacterium. It is one of four species of oral spirochetes to be reliably cultured, the others being Treponema pectinovorum, Treponema socranskii and Treponema vincentii. T. denticola dwells in a complex and diverse microbial community within the oral cavity and is highly specialized to survive in this environment. T. denticola is associated with the incidence and severity of human periodontal disease. Treponema denticola is one of three bacteria that form the Red Complex, the other two being Porphyromonas gingivalis and Tannerella forsythia. Together they form the major virulent pathogens that cause chronic periodontitis. Having elevated T. denticola levels in the mouth is considered one of the main etiological agents of periodontitis. T. denticola is related to the syphilis-causing obligate human pathogen, Treponema pallidum subsp. pallidum. It has also been isolated from women with bacterial vaginosis.
A nontreponemal test (NTT) is a blood test for diagnosis of infection with syphilis. Nontreponemal tests are an indirect method in that they detect biomarkers that are released during cellular damage that occurs from the syphilis spirochete. In contrast, treponemal tests look for antibodies that are a direct result of the infection thus, anti-treponeme IgG, IgM and to a lesser degree IgA. Nontreponemal tests are screening tests, very rapid and relatively simple, but need to be confirmed by treponemal tests. Centers for Disease Control and Prevention (CDC)-approved standard tests include the VDRL test, the rapid plasma reagin (RPR) test, the unheated serum reagin (USR) test, and the toluidine red unheated serum test (TRUST). These have mostly replaced the first nontreponemal test, the Wassermann test.

Pyrotherapy is a method of treatment by raising the body temperature or sustaining an elevated body temperature using a fever. In general, the body temperature was maintained at 41 °C (105 °F). Many diseases were treated by this method in the first half of the 20th century. In general, it was done by exposing the patient to hot baths, warm air, or (electric) blankets. The technique reached its peak of sophistication in the early 20th century with malariotherapy, in which Plasmodium vivax, a causative agent of malaria, was allowed to infect already ill patients in order to produce intense fever for therapeutic ends. The sophistication of this approach lay in using effective anti-malarial drugs to control the P. vivax infection, while maintaining the fever it causes to the detriment of other, ongoing, and then-incurable infections present in the patient, such as late-stage syphilis. This type of pyrotherapy was most famously used by psychiatrist Julius Wagner-Jauregg, who won the Nobel Prize for Medicine in 1927 for his elaboration of the procedure in treating neurosyphilitics.

The Treponema pallidum particle agglutination assay is an indirect agglutination assay used for detection and titration of antibodies against the causative agent of syphilis, Treponema pallidum subspecies pallidum. It also detects other treponematoses.

The first recorded outbreak of syphilis in Europe occurred in 1494/1495 in Naples, Italy, during a French invasion. Because it was spread geographically by French troops returning from that campaign, the disease was known as "French disease", and it was not until 1530 that the term "syphilis" was first applied by the Italian physician and poet Girolamo Fracastoro. The causative organism, Treponema pallidum, was first identified by Fritz Schaudinn and Erich Hoffmann in 1905 at the Charité Clinic in Berlin. The first effective treatment, Salvarsan, was developed in 1910 by Sahachiro Hata in the laboratory of Paul Ehrlich. It was followed by the introduction of penicillin in 1943.