Related Research Articles
Forensic psychiatry is a subspeciality of psychiatry and is related to criminology. It encompasses the interface between law and psychiatry. According to the American Academy of Psychiatry and the Law, it is defined as "a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts involving civil, criminal, correctional, regulatory, or legislative matters, and in specialized clinical consultations in areas such as risk assessment or employment." A forensic psychiatrist provides services – such as determination of competency to stand trial – to a court of law to facilitate the adjudicative process and provide treatment, such as medications and psychotherapy, to criminals.

The Institute of Mental Health (IMH), formerly known as Woodbridge Hospital, is a psychiatric hospital in Hougang, Singapore.
Psychiatric nursing or mental health nursing is the appointed position of a nurse that specialises in mental health, and cares for people of all ages experiencing mental illnesses or distress. These include: neurodevelopmental disorders, schizophrenia, schizoaffective disorder, mood disorders, addiction, anxiety disorders, personality disorders, eating disorders, suicidal thoughts, psychosis, paranoia, and self-harm.
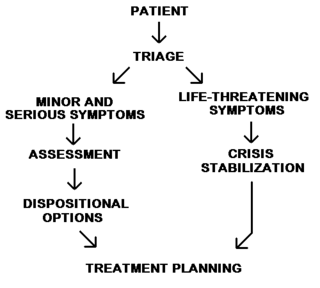
Emergency psychiatry is the clinical application of psychiatry in emergency settings. Conditions requiring psychiatric interventions may include attempted suicide, substance abuse, depression, psychosis, violence or other rapid changes in behavior.
Nursing in the United Kingdom has a long history. The current form of nursing is often considered as beginning with Florence Nightingale who pioneered modern nursing. Nightingale initiated formal schools of nursing in the United Kingdom in the late 19th and early 20th centuries. The role and perception of nursing has dramatically changed from that of a handmaiden to the doctor to professionals in their own right. There are over 700,000 nurses in the United Kingdom and they work in a variety of settings, such as hospitals, health centres, nursing homes, hospices, communities, military, prisons, and academia, with most working for the National Health Service (NHS). Nurses work across all demographics and requirements of the public: adults, children, mental health, and learning disability. Nurses work in a range of specialties from the broad areas of medicine, surgery, theatres, and investigative sciences such as imaging. Nurses also work in large areas of sub-specialities such as respiratory, diabetes, cancer, neurology, infectious diseases, liver, research, cardiac, women's health, sexual health, emergency and acute care, gastrointestinal, infection prevention and control, neuroscience, ophthalmic, pain and palliative, and rheumatology. Nurses often work in multi-disciplinary teams but increasingly are found working independently.
Psychiatric and mental health nurses in the U.S. Army Nurse Corps employing groundbreaking protocols and treatments in psychiatric issues to address the unique challenges that our service men and women face, more commonly post-traumatic stress disorder and traumatic brain injuries. Most people understand that trauma exposure is a popular occupational hazard for military members. Psychiatric screenings, before and during their enlistment, and treatments after being exposed to warfare, death, destruction, and torture have been extremely beneficial for military personnel and their dependents.

Telepsychiatry or telemental health refers to the use of telecommunications technology to deliver psychiatric care remotely for people with mental health conditions. It is a branch of telemedicine.
A mental health professional is a health care practitioner or social and human services provider who offers services for the purpose of improving an individual's mental health or to treat mental disorders. This broad category was developed as a name for community personnel who worked in the new community mental health agencies begun in the 1970s to assist individuals moving from state hospitals, to prevent admissions, and to provide support in homes, jobs, education, and community. These individuals were the forefront brigade to develop the community programs, which today may be referred to by names such as supported housing, psychiatric rehabilitation, supported or transitional employment, sheltered workshops, supported education, daily living skills, affirmative industries, dual diagnosis treatment, individual and family psychoeducation, adult day care, foster care, family services and mental health counseling.
People with schizophrenia are at a higher than average risk of physical ill health, and earlier death than the general population. The fatal conditions include cardiovascular, respiratory and metabolic disorders.
In the United States, a psychiatric-mental health nurse practitioner (PMHNP) is an advanced practice registered nurse trained to provide a wide range of mental health services to patients and families in a variety of settings. PMHNPs diagnose, conduct therapy, and prescribe medications for patients who have psychiatric disorders, medical organic brain disorders or substance abuse problems. They are licensed to provide emergency psychiatric services, psychosocial and physical assessment of their patients, treatment plans, and manage patient care. They may also serve as consultants or as educators for families and staff. The PMHNP has a focus on psychiatric diagnosis, including the differential diagnosis of medical disorders with psychiatric symptoms, and on medication treatment for psychiatric disorders.
Psychoeducation is an evidence-based therapeutic intervention for patients and their loved ones that provides information and support to better understand and cope with illness. Psychoeducation is most often associated with serious mental illness, including dementia, schizophrenia, clinical depression, anxiety disorders, eating disorders, bipolar and personality disorders. The term has also been used for programs that address physical illnesses, such as cancer.
A registered psychiatric nurse (RPN) specialises in a field of nursing that focuses on the mental health of patients. Psychiatric nurses assist the interdisciplinary team in the assessment and treatment of the patient's psychiatric illness and symptoms. They treat a variety of mental health disorders such as bipolar, depression, schizophrenia, anxiety, substance abuse addiction and eating disorders such as bulimia and anorexia. However, they do not diagnose the patient, this is the responsibility of a qualified psychologist or a psychiatric doctor. Psychiatric nurses are in charge of dispensing medication and the overall care of patients. Registered psychiatric nurses work under the supervision of doctors’ and they practice within the health care industry, mostly in mental health clinics, outpatient facilities, mental health agencies, long-term care centres or hospitals.
A psychiatric assessment, or psychological screening, is the process of gathering information about a person within a psychiatric service, with the purpose of making a diagnosis. The assessment is usually the first stage of a treatment process, but psychiatric assessments may also be used for various legal purposes. The assessment includes social and biographical information, direct observations, and data from specific psychological tests. It is typically carried out by a psychiatrist, but it can be a multi-disciplinary process involving nurses, psychologists, occupational therapist, social workers, and licensed professional counselors.

Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses can be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialties with differing levels of prescription authority. Nurses comprise the largest component of most healthcare environments; but there is evidence of international shortages of qualified nurses. Nurses collaborate with other healthcare providers such as physicians, nurse practitioners, physical therapists, and psychologists. There is a distinction between nurses and nurse practitioners; in the U.S., the latter are nurses with a graduate degree in advanced practice nursing, and are permitted to prescribe medications unlike the former. They practice independently in a variety of settings in more than half of the United States. Since the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Psychiatric Intensive Care Units or PICUs are specialist twenty-four hour inpatient wards that provide intensive assessment and comprehensive treatment to individuals during the most acute phase of a serious mental illness.
Psychiatric intensive care is for patients who are in an acutely disturbed phase of a serious mental disorder. There is an associated loss of capacity for self-control with a corresponding increase in risk which does not allow their safe, therapeutic management and treatment in a less acute or a less secure mental health ward. Care and treatment must be patient-centred, multidisciplinary, intensive and have an immediacy of response to critical clinical and risk situations. Patients should be detained compulsorily under the appropriate mental health legislative framework, and the clinical and risk profile of the patient usually requires an associated level of security. Psychiatric intensive care is delivered by qualified and suitably trained multidisciplinary clinicians according to an agreed philosophy of unit operational policy underpinned by the principles of therapeutic intervention and dynamic clinically focused risk management
Kevin Joseph Michael Gournay CBE FMedSci FRCN FRSM FRCPsych (Hon) PhD RN CSci Cert CBT is a registered psychologist, chartered scientist and a registered nurse by background. He is an emeritus professor at the Institute of Psychiatry, King's College London. He was a consultant psychologist at the Priory Hospital North London; retiring in December 2018. He has now returned to clinical work as part of the response to COVID19. He is currently an Honorary Professor at the Matilda Centre; University of Sydney., where his work focusses on the impact of COVID19 on mental health and the combination of mental health problems and substance use. He has been responsible over many years for a very wide range of research, policy and practice development in mental health care. He also works as an Expert Witness; he has provided reports on more than 300 suicides; 20 homicides and hundreds of reports on people who have suffered the consequences of traumatic events, including accidents, terrorist related incidents, natural disasters, war related events and stillbirth and perinatal death. He has also provided numerous reports on patients receiving care and treatment in high secure and Medium secure settings, including Broadmoor, Rampton and Ashworth hospitals
Unlicensed assistive personnel (UAP) are paraprofessionals who assist individuals with physical disabilities, mental impairments, and other health care needs with their activities of daily living (ADLs). UAPs also provide bedside care—including basic nursing procedures—all under the supervision of a registered nurse, licensed practical nurse or other health care professional. UAPs must demonstrate their ability and competence before gaining any expanded responsibilities in a clinical setting. While providing this care, UAPs offer compassion and patience and are part of the patient's healthcare support system. Communication between UAPs and registered nurses (RNs) is key as they are working together in their patients' best interests. The scope of care UAPs are responsible for is delegated by RNs or other clinical licensed professionals.
Covert medication, the covert administration of medicines is when medicines are administered in a disguised form, usually in food or drink, without the knowledge or consent of the individual receiving the drug. The decision-making processes surrounding covert medication should be in the best interests of the patient, transparent and inclusive.
Electroconvulsive therapy (ECT) is a controversial therapy used to treat certain mental illnesses such as major depressive disorder, schizophrenia, depressed bipolar disorder, manic excitement, and catatonia. These disorders are difficult to live with and often very difficult to treat, leaving individuals suffering for long periods of time. In general, ECT is not looked at as a first line approach to treating a mental disorder, but rather a last resort treatment when medications such as antidepressants are not helpful in reducing the clinical manifestations.

Correctional nursing or forensic nursing is nursing as it relates to prisoners. Nurses are required in prisons, jails, and detention centers; their job is to provide physical and mental healthcare for detainees and inmates. In these correctional settings, nurses are the primary healthcare providers. These nurses also work with crime victims and assist in expert witness testimonies, and are involved in a variety of legal cases, including paternity disputes and workplace injuries.
References
- ↑ "Mental health nursing - NHS Careers". National Health Service . Retrieved 3 January 2015.
- 1 2 3 4 "Mental health nurse: Job description". Prospects. Retrieved 4 February 2016.
- 1 2 "Workforce planning in the NHS". The King's Fund. 29 April 2015. Retrieved 2016-02-04.
- ↑ International Journal of Nursing Studies. Volume 44, Issue 3, March 2007, Pages 479–509. MENTAL HEALTH SPECIAL ISSUE. Systematic review of interventions delivered by UK mental health nurses. Joseph Currana, Charles Brookerb
- ↑ JONES, A. and JONES, M. (2005), Mental health nurse prescribing: issues for the UK. Journal of Psychiatric and Mental Health Nursing, 12: 527–535. doi : 10.1111/j.1365-2850.2005.00857.x
- ↑ Kevin Gourney (1996) Advances in Psychiatric Treatment, mental health nursing: issues and roles. vol.2, pp.W3-W9
- ↑ Allebeck P., (1989). Schizophrenia: a life- shortening disease. Schizophrenia Bulletin, 15, 81-89
- ↑ Richard IG Holt. Cardiovascular disease and diabetes in people with severe mental illness: causes, consequences and pragmatic management. doi : 10.3132/pccj.2011.085
- ↑ Brady S. M. and Carmen E: AIDS risk in the chronically mentally ill: clinical strategies for prevention. New Directions for Mental Health Services, 48, 83-95, 1990 -9