Related Research Articles

Contact lenses, or simply contacts, are thin lenses placed directly on the surface of the eyes. Contact lenses are ocular prosthetic devices used by over 150 million people worldwide, and they can be worn to correct vision or for cosmetic or therapeutic reasons. In 2010, the worldwide market for contact lenses was estimated at $6.1 billion, while the US soft lens market was estimated at $2.1 billion. Multiple analysts estimated that the global market for contact lenses would reach $11.7 billion by 2015. As of 2010, the average age of contact lens wearers globally was 31 years old, and two-thirds of wearers were female.
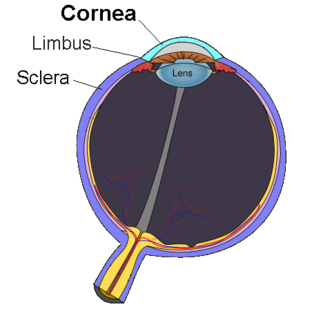
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Along with the anterior chamber and lens, the cornea refracts light, accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.

Keratitis is a condition in which the eye's cornea, the clear dome on the front surface of the eye, becomes inflamed. The condition is often marked by moderate to intense pain and usually involves any of the following symptoms: pain, impaired eyesight, photophobia, red eye and a 'gritty' sensation.

Eye surgery, also known as ophthalmic or ocular surgery, is surgery performed on the eye or its adnexa, by an ophthalmologist. Eye surgery is synonymous with ophthalmology. The eye is a very fragile organ, and requires extreme care before, during, and after a surgical procedure to minimize or prevent further damage. An expert eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts dating back as early as 1800 BC, with cataract treatment starting in the fifth century BC. Today it continues to be a widely practiced type of surgery, with various techniques having been developed for treating eye problems.

Phacoemulsification is a modern cataract surgery method in which the eye's internal lens is emulsified with an ultrasonic handpiece and aspirated from the eye. Aspirated fluids are replaced with irrigation of balanced salt solution to maintain the anterior chamber.

Dry eye syndrome (DES), also known as keratoconjunctivitis sicca (KCS), is the condition of having dry eyes. Other associated symptoms include irritation, redness, discharge, and easily fatigued eyes. Blurred vision may also occur. Symptoms range from mild and occasional to severe and continuous. Scarring of the cornea may occur in untreated cases.

Cataract surgery, also called lens replacement surgery, is the removal of the natural lens of the eye that has developed an opacification, which is referred to as a cataract, and its replacement with an intraocular lens. Metabolic changes of the crystalline lens fibers over time lead to the development of the cataract, causing impairment or loss of vision. Some infants are born with congenital cataracts, and certain environmental factors may also lead to cataract formation. Early symptoms may include strong glare from lights and small light sources at night, and reduced acuity at low light levels.

Physical or chemical injuries of the eye can be a serious threat to vision if not treated appropriately and in a timely fashion. The most obvious presentation of ocular (eye) injuries is redness and pain of the affected eyes. This is not, however, universally true, as tiny metallic projectiles may cause neither symptom. Tiny metallic projectiles should be suspected when a patient reports metal on metal contact, such as with hammering a metal surface. Corneal foreign body is one of the most common preventable occupational hazard. Intraocular foreign bodies do not cause pain because of the lack of nerve endings in the vitreous humour and retina that can transmit pain sensations. As such, general or emergency department doctors should refer cases involving the posterior segment of the eye or intraocular foreign bodies to an ophthalmologist. Ideally, ointment would not be used when referring to an ophthalmologist, since it diminishes the ability to carry out a thorough eye examination.

Corneal abrasion is a scratch to the surface of the cornea of the eye. Symptoms include pain, redness, light sensitivity, and a feeling like a foreign body is in the eye. Most people recover completely within three days.

A scleral lens, also known as a scleral contact lens, is a large contact lens that rests on the sclera and creates a tear-filled vault over the cornea. Scleral lenses are designed to treat a variety of eye conditions, many of which do not respond to other forms of treatment.

Acanthamoeba keratitis (AK) is a rare disease in which amoebae of the genus Acanthamoeba invade the clear portion of the front (cornea) of the eye. It affects roughly 100 people in the United States each year. Acanthamoeba are protozoa found nearly ubiquitously in soil and water and can cause infections of the skin, eyes, and central nervous system.
Fungal keratitis is a fungal infection of the cornea, which can lead to blindness. It generally presents with a red, painful eye and blurred vision. There is also increased sensitivity to light, and excessive tears or discharge.
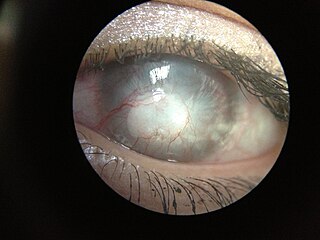
Corneal neovascularization (CNV) is the in-growth of new blood vessels from the pericorneal plexus into avascular corneal tissue as a result of oxygen deprivation. Maintaining avascularity of the corneal stroma is an important aspect of corneal pathophysiology as it is required for corneal transparency and optimal vision. A decrease in corneal transparency causes visual acuity deterioration. Corneal tissue is avascular in nature and the presence of vascularization, which can be deep or superficial, is always pathologically related.
Loran B. Morgan was a United States ophthalmologist best known as the inventor of the Morgan Lens.

Herpetic simplex keratitis is a form of keratitis caused by recurrent herpes simplex virus (HSV) infection in the cornea.

Ophthalmic drug administration is the administration of a drug to the eyes, most typically as an eye drop formulation. Topical formulations are used to combat a multitude of diseased states of the eye. These states may include bacterial infections, eye injury, glaucoma, and dry eye. However, there are many challenges associated with topical delivery of drugs to the cornea of the eye.

Phacolytic glaucoma (PG) is a form of glaucoma which is caused due to a leaking mature or immature cataract. Inflammatory glaucoma which occurs in phacolysis is a condition which is a result of the leakage of protein within the lens into the capsule of a mature or hyper mature cataract and involves a simple procedure to be cured that is referred to as cataract extraction.
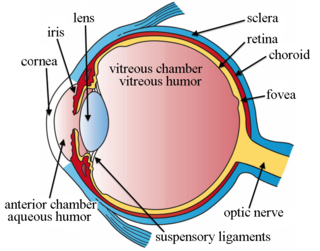
Intravitreal injection is the method of administration of drugs into the eye by injection with a fine needle. The medication will be directly applied into the vitreous humor. It is used to treat various eye diseases, such as age-related macular degeneration (AMD), diabetic retinopathy, and infections inside the eye such as endophthalmitis. As compared to topical administration, this method is beneficial for a more localized delivery of medications to the targeted site, as the needle can directly pass through the anatomical eye barrier and dynamic barrier. It could also minimize adverse drug effect to other body tissues via the systemic circulation, which could be a possible risk for intravenous injection of medications. Although there are risks of infections or other complications, with suitable precautions throughout the injection process, chances for these complications could be lowered.
Exposure keratopathy is medical condition affecting the cornea of eyes. It can lead to corneal ulceration and permanent loss of vision due to corneal opacity.
Peripheral Ulcerative Keratitis (PUK) is a group of destructive inflammatory diseases involving the peripheral cornea in human eyes. The symptoms of PUK include pain, redness of the eyeball, photophobia, and decreased vision accompanied by distinctive signs of crescent-shaped damage of the cornea. The causes of this disease are broad, ranging from injuries, contamination of contact lenses, to association with other systemic conditions. PUK is associated with different ocular and systemic diseases. Mooren's ulcer is a common form of PUK. The majority of PUK is mediated by local or systemic immunological processes, which can lead to inflammation and eventually tissue damage. Standard PUK diagnostic test involves reviewing the medical history and a completing physical examinations. Two major treatments are the use of medications such as corticosteroids or other immunosuppressive agents and surgical resection of the conjunctiva. The prognosis of PUK is unclear with one study providing potential complications. PUK is a rare condition with an estimated incidence of 3 per million annually.
References
- 1 2 3 4 Home page of www.morganlens.com
- 1 2 3 Zeke Scher, "The Wyoming Doctor Who Saves Eyes", Denver Post, Feb. 20, 1972 Archived 2008-08-20 at the Wayback Machine
- 1 2 3 4 5 6 FAQs from Morgan Lens website Archived 2012-06-19 at the Wayback Machine
- 1 2 3 Oregon Health Dept. guide to Morgan Lens
- ↑ PowerPoint presentation from Morgan Lens' manufacturer
- ↑ Home page of www.morganlens.com, Profile of MorTan, Inc. on healthcare.zibb.com
- ↑ Profile from zapconnect.com