A nerve is an enclosed, cable-like bundle of nerve fibers in the peripheral nervous system.

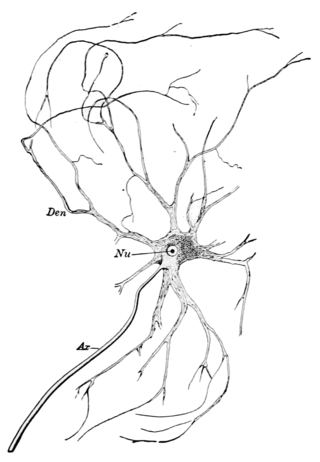
Nervous tissue, also called neural tissue, is the main tissue component of the nervous system. The nervous system regulates and controls body functions and activity. It consists of two parts: the central nervous system (CNS) comprising the brain and spinal cord, and the peripheral nervous system (PNS) comprising the branching peripheral nerves. It is composed of neurons, also known as nerve cells, which receive and transmit impulses to and from it, and neuroglia, also known as glial cells or glia, which assist the propagation of the nerve impulse as well as provide nutrients to the neurons.
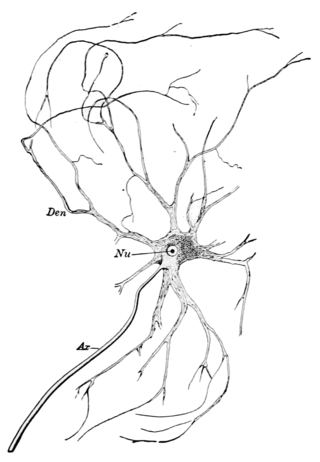
A motor nerve, or efferent nerve, is a nerve that contains exclusively efferent nerve fibers and transmits motor signals from the central nervous system (CNS) to the muscles of the body. This is different from the motor neuron, which includes a cell body and branching of dendrites, while the nerve is made up of a bundle of axons. Motor nerves act as efferent nerves which carry information out from the CNS to muscles, as opposed to afferent nerves, which transfer signals from sensory receptors in the periphery to the CNS. Efferent nerves can also connect to glands or other organs/issues instead of muscles. The vast majority of nerves contain both sensory and motor fibers and are therefore called mixed nerves.

Wallerian degeneration is an active process of degeneration that results when a nerve fiber is cut or crushed and the part of the axon distal to the injury degenerates. A related process of dying back or retrograde degeneration known as 'Wallerian-like degeneration' occurs in many neurodegenerative diseases, especially those where axonal transport is impaired such as amyotrophic lateral sclerosis (ALS) and Alzheimer's disease. Primary culture studies suggest that a failure to deliver sufficient quantities of the essential axonal protein NMNAT2 is a key initiating event.
Electroneuronography or electroneurography (ENoG) is a neurological non-invasive test used to study the facial nerve in cases of muscle weakness in one side of the face. The technique of electroneuronography was first used by Esslen and Fisch in 1979 to describe a technique that examines the integrity and conductivity of peripheral nerves. In modern use, ENoG is used to describe study of the facial nerve, while the term nerve conduction study is employed for other nerves.
Neurotmesis is part of Seddon's classification scheme used to classify nerve damage. It is the most serious nerve injury in the scheme. In this type of injury, both the nerve and the nerve sheath are disrupted. While partial recovery may occur, complete recovery is impossible.
Axonotmesis is an injury to the peripheral nerve of one of the extremities of the body. The axons and their myelin sheath are damaged in this kind of injury, but the endoneurium, perineurium and epineurium remain intact. Motor and sensory functions distal to the point of injury are completely lost over time leading to Wallerian degeneration due to ischemia, or loss of blood supply. Axonotmesis is usually the result of a more severe crush or contusion than neurapraxia.
Neurapraxia is a disorder of the peripheral nervous system in which there is a temporary loss of motor and sensory function due to blockage of nerve conduction, usually lasting an average of six to eight weeks before full recovery. Neurapraxia is derived from the word apraxia, meaning “loss or impairment of the ability to execute complex coordinated movements without muscular or sensory impairment”.
Neuralgia is pain in the distribution of a nerve or nerves, as in intercostal neuralgia, trigeminal neuralgia, and glossopharyngeal neuralgia.
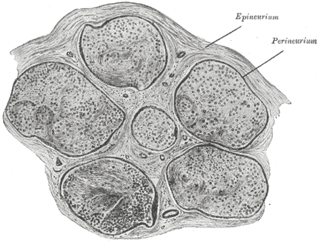
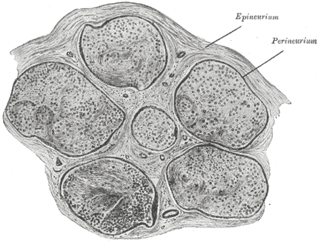
The epineurium is the outermost layer of dense irregular connective tissue surrounding a peripheral nerve. It usually surrounds multiple nerve fascicles as well as blood vessels which supply the nerve. Smaller branches of these blood vessels penetrate into the perineurium. In addition to blood vessels which supply the nerve, lymphocytes and fibroblasts are also present and contribute to the production of collagen fibers that form the backbone of the epineurium. In addition to providing structural support, lymphocytes and fibroblasts also play a vital role in maintenance and repair of the surrounding tissues.

A brachial plexus injury (BPI), also known as brachial plexus lesion, is an injury to the brachial plexus, the network of nerves that conducts signals from the spinal cord to the shoulder, arm and hand. These nerves originate in the fifth, sixth, seventh and eighth cervical (C5–C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand.
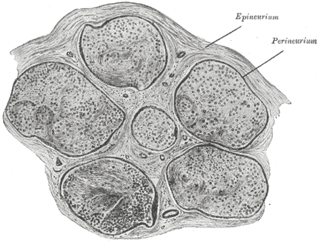
The perineurium is a protective sheath that surrounds a nerve fascicle. This bundles together axons targeting the same anatomical location. The perineurium is composed from fibroblasts.
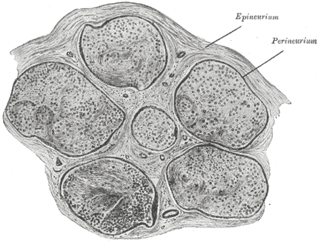
The endoneurium is a layer of delicate connective tissue around the myelin sheath of each myelinated nerve fiber in the peripheral nervous system. Its component cells are called endoneurial cells. The endoneuria with their enclosed nerve fibers are bundled into groups called nerve fascicles, each fascicle within its own protective sheath called a perineurium. In sufficiently large nerves multiple fascicles, each with its blood supply and fatty tissue, may be bundled within yet another sheath, the epineurium.

Nerve injury is an injury to a nerve. There is no single classification system that can describe all the many variations of nerve injuries. In 1941, Seddon introduced a classification of nerve injuries based on three main types of nerve fiber injury and whether there is continuity of the nerve. Usually, however, nerve injuries are classified in five stages, based on the extent of damage to both the nerve and the surrounding connective tissue, since supporting glial cells may be involved.
Neuroregeneration is the regrowth or repair of nervous tissues, cells or cell products. Neuroregenerative mechanisms may include generation of new neurons, glia, axons, myelin, or synapses. Neuroregeneration differs between the peripheral nervous system (PNS) and the central nervous system (CNS) by the functional mechanisms involved, especially in the extent and speed of repair. When an axon is damaged, the distal segment undergoes Wallerian degeneration, losing its myelin sheath. The proximal segment can either die by apoptosis or undergo the chromatolytic reaction, which is an attempt at repair. In the CNS, synaptic stripping occurs as glial foot processes invade the dead synapse.
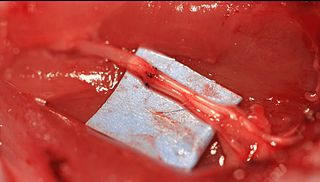
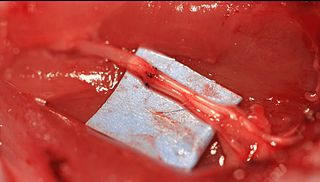
Epineurial repair is a common surgical procedure to repair a nerve laceration via the epineurium, the connective tissue surrounding nerve fibers originating from the spinal cord. It is intended to allow the restoration of sensory function. When a nerve is lacerated or cut, repair is done by sewing the cut ends together through the epineurium to increase the potential of the proximal part growing correctly along the route the degrading distal part leaves behind. Usual sensation and mobility will not be an immediate result because nerves grow at a rate of approximately 1 millimeter per day, so it will take a few months to notice the final outcome. Research in use of nerve grafts and nerve growth factors is being done to speed recovery time.
Nerve allotransplantation is the transplantation of a nerve to a receiver from a donor of the same species. For example, nerve tissue is transplanted from one person to another. Allotransplantation is a commonly used type of transplantation of which nerve repair is one specific aspect.
Cryoneurolysis, also referred to as cryoanalgesia, is a medical procedure that temporarily blocks nerve conduction along peripheral nerve pathways. The procedure, which inserts a small probe to freeze the target nerve, can facilitate complete regeneration of the structure and function of the affected nerve. Cryoneurolysis has been used to treat a variety of painful conditions.
Facial nerve decompression is a type of nerve decompression surgery where abnormal compression on the facial nerve is relieved.

Nerve entrapment involves a cascade of physiological changes caused by compression and tension. Some of these changes are irreversible. The magnitude and duration of the forces determines the extent of injury. In the acute form, mechanical injury and metabolic blocks impede nerve function. In the chronic form, there is a sequence of changes starting with a breakdown of the blood-nerve-barrier, followed by edema with connective tissue changes, followed by diffuse demyelination, and finally followed by axonmetesis. The injury will often be a mixed lesion where mild/moderate compression is a combination of a metabolic block and neuropraxia, while severe compression combines elements of neuropraxia and axonmetesis.