Related Research Articles

Allergies, also known as allergic diseases, are various conditions caused by hypersensitivity of the immune system to typically harmless substances in the environment. These diseases include hay fever, food allergies, atopic dermatitis, allergic asthma, and anaphylaxis. Symptoms may include red eyes, an itchy rash, sneezing, coughing, a runny nose, shortness of breath, or swelling. Note that food intolerances and food poisoning are separate conditions.
An allergen is an otherwise harmless substance that triggers an allergic reaction in sensitive individuals by stimulating an immune response.

A podiatrist is a medical professional devoted to the treatment of disorders of the foot, ankle, and related structures of the leg. The term originated in North America but has now become the accepted term in the English-speaking world for all practitioners of podiatric medicine. The word chiropodist was previously used in the United States, but it is now regarded as antiquated.
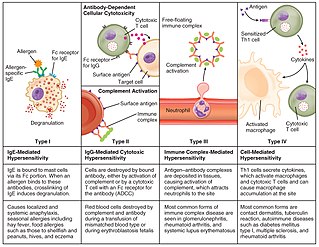
Hypersensitivity is an abnormal physiological condition in which there is an undesirable and adverse immune response to an antigen. It is an abnormality in the immune system that causes immune diseases including allergies and autoimmunity. It is caused by many types of particles and substances from the external environment or from within the body that are recognized by the immune cells as antigens. The immune reactions are usually referred to as an over-reaction of the immune system and they are often damaging and uncomfortable.

A nail disease or onychosis is a disease or deformity of the nail. Although the nail is a structure produced by the skin and is a skin appendage, nail diseases have a distinct classification as they have their own signs and symptoms which may relate to other medical conditions. Some nail conditions that show signs of infection or inflammation may require medical assistance.

Rhinitis, also known as coryza, is irritation and inflammation of the mucous membrane inside the nose. Common symptoms are a stuffy nose, runny nose, sneezing, and post-nasal drip.

Athlete's foot, known medically as tinea pedis, is a common skin infection of the feet caused by a fungus. Signs and symptoms often include itching, scaling, cracking and redness. In rare cases the skin may blister. Athlete's foot fungus may infect any part of the foot, but most often grows between the toes. The next most common area is the bottom of the foot. The same fungus may also affect the nails or the hands. It is a member of the group of diseases known as tinea.
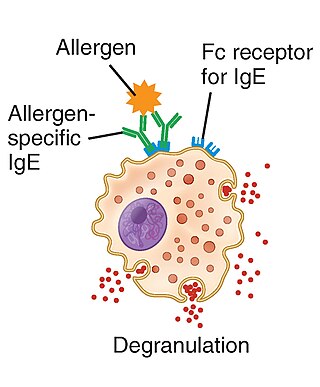
Type I hypersensitivity, in the Gell and Coombs classification of allergic reactions, is an allergic reaction provoked by re-exposure to a specific type of antigen referred to as an allergen. Type I is distinct from type II, type III and type IV hypersensitivities. The relevance of the Gell and Coombs classification of allergic reactions has been questioned in the modern-day understanding of allergy, and it has limited utility in clinical practice.
Dermatophyte is a common label for a group of fungus of Arthrodermataceae that commonly causes skin disease in animals and humans. Traditionally, these anamorphic mold genera are: Microsporum, Epidermophyton and Trichophyton. There are about 40 species in these three genera. Species capable of reproducing sexually belong in the teleomorphic genus Arthroderma, of the Ascomycota. As of 2019 a total of nine genera are identified and new phylogenetic taxonomy has been proposed.

Atopy is the tendency to produce an exaggerated immunoglobulin E (IgE) immune response to otherwise harmless substances in the environment. Allergic diseases are clinical manifestations of such inappropriate, atopic responses.

Rhinorrhea, also spelled rhinorrhoea or rhinorrhœa, or informally runny nose is the free discharge of a thin mucus fluid from the nose; it is a common condition. It is a common symptom of allergies or certain viral infections, such as the common cold or COVID-19. It can be a side effect of crying, exposure to cold temperatures, cocaine abuse, or drug withdrawal, such as from methadone or other opioids. Treatment for rhinorrhea may be aimed at reducing symptoms or treating underlying causes. Rhinorrhea usually resolves without intervention, but may require treatment by a doctor if symptoms last more than 10 days or if symptoms are the result of foreign bodies in the nose.

Dermatophytosis, also known as tinea and ringworm, is a fungal infection of the skin, that may affect skin, hair, and nails. Typically it results in a red, itchy, scaly, circular rash. Hair loss may occur in the area affected. Symptoms begin four to fourteen days after exposure. The types of dermatophytosis are typically named for area of the body that they affect. Multiple areas can be affected at a given time.

Onychomycosis, also known as tinea unguium, is a fungal infection of the nail. Symptoms may include white or yellow nail discoloration, thickening of the nail, and separation of the nail from the nail bed. Fingernails may be affected, but it is more common for toenails. Complications may include cellulitis of the lower leg. A number of different types of fungus can cause onychomycosis, including dermatophytes and Fusarium. Risk factors include athlete's foot, other nail diseases, exposure to someone with the condition, peripheral vascular disease, and poor immune function. The diagnosis is generally suspected based on the appearance and confirmed by laboratory testing.
Occupational lung diseases comprise a broad group of diseases, including occupational asthma, industrial bronchitis, chronic obstructive pulmonary disease (COPD), bronchiolitis obliterans, inhalation injury, interstitial lung diseases, infections, lung cancer and mesothelioma. These can be caused directly or due to immunological response to an exposure to a variety of dusts, chemicals, proteins or organisms. Occupational cases of interstitial lung disease may be misdiagnosed as COPD, idiopathic pulmonary fibrosis, or a myriad of other diseases; leading to a delay in identification of the causative agent.

Allergic inflammation is an important pathophysiological feature of several disabilities or medical conditions including allergic asthma, atopic dermatitis, allergic rhinitis and several ocular allergic diseases. Allergic reactions may generally be divided into two components; the early phase reaction, and the late phase reaction. While the contribution to the development of symptoms from each of the phases varies greatly between diseases, both are usually present and provide us a framework for understanding allergic disease.

Trichophyton rubrum is a dermatophytic fungus in the phylum Ascomycota. It is an exclusively clonal, anthropophilic saprotroph that colonizes the upper layers of dead skin, and is the most common cause of athlete's foot, fungal infection of nail, jock itch, and ringworm worldwide. Trichophyton rubrum was first described by Malmsten in 1845 and is currently considered to be a complex of species that comprises multiple, geographically patterned morphotypes, several of which have been formally described as distinct taxa, including T. raubitschekii, T. gourvilii, T. megninii and T. soudanense.

Trichophyton is a genus of fungi, which includes the parasitic varieties that cause tinea, including athlete's foot, ringworm, jock itch, and similar infections of the nail, beard, skin and scalp. Trichophyton fungi are molds characterized by the development of both smooth-walled macro- and microconidia. Macroconidia are mostly borne laterally directly on the hyphae or on short pedicels, and are thin- or thick-walled, clavate to fusiform, and range from 4 to 8 by 8 to 50 μm in size. Macroconidia are few or absent in many species. Microconidia are spherical, pyriform to clavate or of irregular shape, and range from 2 to 3 by 2 to 4 μm in size.

Cochliobolus lunatus is a fungal plant pathogen that can cause disease in humans and other animals. The anamorph of this fungus is known as Curvularia lunata, while C. lunatus denotes the teleomorph or sexual stage. They are, however, the same biological entity. C. lunatus is the most commonly reported species in clinical cases of reported Cochliobolus infection.
Occupational asthma is new onset asthma or the recurrence of previously quiescent asthma directly caused by exposure to an agent at workplace. It is an occupational lung disease and a type of work-related asthma. Agents that can induce occupational asthma can be grouped into sensitizers and irritants.

Occupational dust exposure occurs when small particles are generated at the workplace through the disturbance/agitation of rock/mineral, dry grain, timber, fiber, or other material. When these small particles become suspended in the air, they can pose a risk to the health of those who breath in the contaminated air.
References
- 1 2 3 4 Ward GW, Karlsson G, Rose G, Platts-Mills TAE (1989). "Trichophyton asthma: sensitization of bronchi and upper airways to dermatophytes antigen". Lancet 8643, 859-62
- 1 2 3 Abramson C (1990). "Inhalation of nail dust: A podiatric hazard". In McCarthy DJ, Abramson C, Rupp MJ (eds). Infectious Diseases of the Lower Extremities. Williams & Wilkins, Baltimore 293-298
- ↑ Woodfolk JA (2005). "Allergy and Dermatophytes". Asthma and Allergic Diseases Center, Clinical Microbiology Reviews18 30-43
- 1 2 3 4 McLarnon NA, Burrow JG, Price P, Aidoo KE, MacLaren W, Harper M, Hepher M, Edwards G (2005). "The controls of airborne hazardous substance in the healthcare environment", IOHA Pilannesberg: paper E1-1, 1-6
- 1 2 Gatley M (1991). "Human nail dust: hazard to chiropodists or merely nuisance?" J. Soc. Occup. Med41 (3) 121-5
- ↑ Sehgal VN, Jain S (2000). "Onychomycosis: clinical perspective". International Journal of Dermatology39241-249
- 1 2 http://www.podiatrytoday.com/article/775 7/5/07
- 1 2 Abramson C and Wilton J (1985). "Inhalation of nail dust aerosols during reduction of onychomycotic toenails: I. Characterization of nail dust particles". JAPMA75563 111-115
- 1 2 3 Harvey CK (1993). "Comparison of the effectiveness of nail dust extractors". Journal of American Podiatric Medical Association833. 12 669-673
- ↑ (2003) "Adverse Human Health Effects Associated with Molds in the Indoor Environment". Journal of Occupational and Environmental Medicine45(5) 470-478
- ↑ Pugh J, Skone JF (1972) "The health of the chiropodist in a developing community service". The Chiropodist27(2)53-55
- 1 2 3 Davies RR, Ganderton MA (1975) "Allergic hazards in chiropody". Chiropodist30(89) 89-92
- 1 2 Duell B L, Arruda LK, Chapman MD, Platts-Mills TAE (1991). "Trichophyton tonsurans Allergen. Characterization of a protein that causes immediate but not delayed hypersensitivity". Journal of Immunology147 136, 96-101
- ↑ (1991) Medical aspects of occupational asthma. Health and Safety Executive Publications, Medical Series 25 16
- ↑ Millar NA (2000). The ocular risks of human nail dust in podiatry. PhD Thesis, Glasgow Caledonian University
- 1 2 3 4 5 6 Davies RR, Ganderton MA, Savage M (1983). "Human nail dust and precipitating antibodies to Trichophyton rubrum in chiropodists". Clin Allergy13309-315
- 1 2 3 Ward PE (1995). "Atopy and reaction to nail dust inhalation". Clinics in Podiatric Medicine12(2) 275-278
- 1 2 3 Millar NA, Burrow, JG, Hay J, Stevenson R (1996) "Putative risks of ocular infection for chiropodists and podiatrists". Journal of British Podiatric Medicine51(11) 158-160
- 1 2 Abramson, Carl and Wilton, James (1992). "Nail dust aerosols from onychomycotic toenails". Journal of the American Podiatric Medical Association82(2)563-567
- ↑ Kivity S, Schawarz Y, Fireman E (1992). "The association of perennial rhinitis with trichophyton infection". Clinical and Experimental Allergy22(4)498-500
- ↑ Davis JM, Kugler G, Nixon BP (1991). "Eye Injury in a Podiatrist". Journal of the American Podiatric Medical Association81(12)661-663
- ↑ Bell KM, Clement DA (1991). "Eye protection for the surgeon". JR Coll Surg Edinb36178-179
- 1 2 Ward GW, Woodfolk JA, Hayden ML, Jackson S, Platts-Mills TAE (1999). "Treatment of late-onset asthma with fluconazole". J Allergy Clin Immunol104 546-550
- 1 2 Wise F, Sulzberger MB (1930) "Urticaria and hay fever due to Trichophyton". JAMA95 1504
- ↑ Schwartz HJ, Ward GW (1995). "Onychomycosis, trichophyton allergy and asthma – a causal relationship?" Ann Allergy Asthma Immunol 74 523-524
- ↑ Platts-Mills TAE, Fiocco GP, Pollart SM, Hayden ML, Jackson S, Wilkens SR (1986). "Trichophyton allergy in a 24-year-old man with intrinsic asthma". Ann Allergy56 40-45
- ↑ Platts-Mills TAE, Call RS, Deuell BA, Kalsson G, Ward GW (1992). "The association of hypersensitivity diseases with dermatophytes infections". Clin Exp Allergy22427-428
- ↑ Kivity S, Schwarz Y, Fireman E. (1999). "The association of perennial rhinitis with trichophyton infection". Clin Exp Allergy22498-500