An embolism is the lodging of an embolus, a blockage-causing piece of material, inside a blood vessel. The embolus may be a blood clot (thrombus), a fat globule, a bubble of air or other gas, amniotic fluid, or foreign material. An embolism can cause partial or total blockage of blood flow in the affected vessel. Such a blockage may affect a part of the body distant from the origin of the embolus. An embolism in which the embolus is a piece of thrombus is called a thromboembolism.

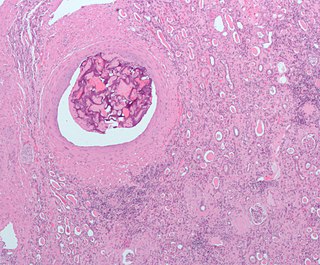
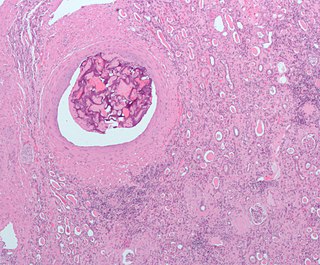
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus.

Venous thrombosis is thrombosis in a vein, caused by a thrombus. A common form of venous thrombosis is deep vein thrombosis (DVT), when a blood clot forms in the deep veins. If a thrombus breaks off (embolizes) and flows towards the lungs, it can become a pulmonary embolism (PE), a blood clot in the lungs. The conditions of DVT only, DVT with PE, and PE only are captured by the term venous thromboembolism (VTE).

The great saphenous vein is a large, subcutaneous, superficial vein of the leg. It is the longest vein in the body, running along the length of the lower limb, returning blood from the foot, leg and thigh to the deep femoral vein at the femoral triangle.

Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.

Deep vein thrombosis (DVT) is the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enlarged veins in the affected area, but some DVTs have no symptoms. The most common life-threatening concern with DVT is the potential for a clot to embolize, travel as an embolus through the right side of the heart, and become lodged in a pulmonary artery that supplies blood to the lungs. This is called a pulmonary embolism (PE). DVT and PE comprise the cardiovascular disease of venous thromboembolism (VTE). About two-thirds of VTE manifests as DVT only, with one-third manifesting as PE with or without DVT. The most frequent long-term DVT complication is post-thrombotic syndrome, which can cause pain, swelling, a sensation of heaviness, itching, and in severe cases, ulcers. Recurrent VTE occurs in about 30% of those in the ten years following an initial VTE.

Budd–Chiari syndrome is a very rare condition, affecting one in a million adults. The condition is caused by occlusion of the hepatic veins that drain the liver. It presents with the classical triad of abdominal pain, ascites, and liver enlargement. The formation of a blood clot within the hepatic veins can lead to Budd–Chiari syndrome. The syndrome can be fulminant, acute, chronic, or asymptomatic. Subacute presentation is the most common form.
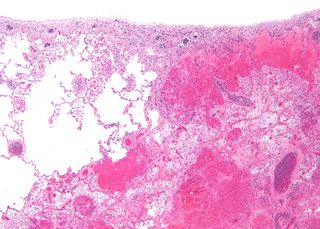
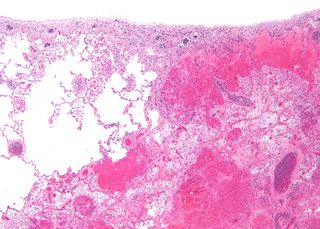
Infarction is tissue death (necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct (from the Latin infarctus, "stuffed into").
A peripheral vascular examination is a medical examination to discover signs of pathology in the peripheral vascular system. It is performed as part of a physical examination, or when a patient presents with leg pain suggestive of a cardiovascular pathology.

Compression stockings are a specialized hosiery designed to help prevent the occurrence of, and guard against further progression of, venous disorders such as edema, phlebitis and thrombosis. Compression stockings are elastic compression garments worn around the leg, compressing the limb. This reduces the diameter of distended veins and increases venous blood flow velocity and valve effectiveness. Compression therapy helps decrease venous pressure, prevents venous stasis and impairments of venous walls, and relieves heavy and aching legs.

Post-thrombotic syndrome (PTS), also called postphlebitic syndrome and venous stress disorder is a medical condition that may occur as a long-term complication of deep vein thrombosis (DVT).

Phlegmasia cerulea dolens (PCD), not to be confused with preceding phlegmasia alba dolens, is an uncommon severe form of lower extremity deep venous thrombosis (DVT) that obstructs blood outflow from a vein. Upper extremity PCD is less common, occurring in under 10% of all cases. PCD results from extensive thrombotic occlusion of extremity veins, most commonly an "iliofemoral" DVT of the iliac vein and/or common femoral vein. It is a medical emergency requiring immediate evaluation and treatment.
The term venous translucence has been used in phlebology since 1996 by surgeon Pedro Fernandes Neto during ambulatory clinical exams in Brazil. His results were published in the annals of the national and international congresses of angiology. Venous translucence is the process of reflective image visualization of veins by light, which reaches up to the superficial venous system. It is a non-invasive method. Since it is a simple, low-cost technique it can be repeated as needed, which is useful in disease-process monitoring. It is a new diagnostic procedure, still undergoing investigation; more analysis is necessary to hone its technical aspects. Venous translucence is based on optical physics. It is caused by the refraction, absorption and reflection of light. The color which is not absorbed is reflected, and is the one that is seen. Therefore, venous translumination is based on the incidence of luminosity on the vein, where part of the light is absorbed and another reflected.

Chronic venous insufficiency (CVI) is a medical condition in which blood pools in the veins, straining the walls of the vein. The most common cause of CVI is superficial venous reflux which is a treatable condition. As functional venous valves are required to provide for efficient blood return from the lower extremities, this condition typically affects the legs. If the impaired vein function causes significant symptoms, such as swelling and ulcer formation, it is referred to as chronic venous disease. It is sometimes called chronic peripheral venous insufficiency and should not be confused with post-thrombotic syndrome in which the deep veins have been damaged by previous deep vein thrombosis.

Central retinal vein occlusion, also CRVO, is when the central retinal vein becomes occluded, usually through thrombosis. The central retinal vein is the venous equivalent of the central retinal artery and both may become occluded. Since the central retinal artery and vein are the sole source of blood supply and drainage for the retina, such occlusion can lead to severe damage to the retina and blindness, due to ischemia and edema (swelling).

Superficial thrombophlebitis is a thrombosis and inflammation of superficial veins which presents as a painful induration with erythema, often in a linear or branching configuration forming cords.

Acute limb ischaemia (ALI) occurs when there is a sudden lack of blood flow to a limb.

Superficial vein thrombosis (SVT) is a blood clot formed in a superficial vein, a vein near the surface of the body. Usually there is thrombophlebitis, which is an inflammatory reaction around a thrombosed vein, presenting as a painful induration with redness. SVT itself has limited significance when compared to a deep vein thrombosis (DVT), which occurs deeper in the body at the deep venous system level. However, SVT can lead to serious complications, and is therefore no longer regarded as a benign condition. If the blood clot is too near the saphenofemoral junction there is a higher risk of pulmonary embolism, a potentially life-threatening complication.