Related Research Articles

Peripheral neuropathy, often shortened to neuropathy, refers to damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerve fibers are affected. Neuropathies affecting motor, sensory, or autonomic nerve fibers result in different symptoms. More than one type of fiber may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.

Polyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.
Tick paralysis is a type of paralysis caused by specific types of attached ticks. Unlike tick-borne diseases caused by infectious organisms, the illness is caused by a neurotoxin produced in the tick's salivary gland. After prolonged attachment, the engorged tick transmits the toxin to its host. The incidence of tick paralysis is unknown. Patients can experience severe respiratory distress.

Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development. This disease typically occurs in chronic alcoholics who have some sort of nutritional deficiency. Treatment may involve nutritional supplementation, pain management, and abstaining from alcohol.
Laryngeal paralysis in animals is a condition in which the nerves and muscles that control the movements of one or both arytenoid cartilages of the larynx cease to function, and instead of opening during aspiration and closing during swallowing, the arytenoids remain stationary in a somewhat neutral position. Specifically, the muscle that causes abduction of the arytenoid cartilage, the cricoarytenoideus dorsalis muscle, ceases to function. This leads to inadequate ventilation during exercise and during thermoregulatory panting as well as incomplete protection of the airway during swallowing.

The health of dogs is a well studied area in veterinary medicine.

Giant axonal neuropathy is a rare, autosomal recessive neurological disorder that causes disorganization of neurofilaments. Neurofilaments form a structural framework that helps to define the shape and size of neurons and are essential for normal nerve function. A distinguishing feature is its association with kinky, or curly, hair; in such cases it has been called Giant axonal neuropathy with curly hair.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.

Lymphoma (lymphosarcoma) in animals is a type of cancer defined by a proliferation of malignant lymphocytes within solid organs such as the lymph nodes, bone marrow, liver and spleen. The disease also may occur in the eye, skin, and gastrointestinal tract.
Scottie Cramp is a disease in Scottish Terriers causing spasms and hyperflexion and hyperextension of the legs. It is caused by a disorder in serotonin metabolism that causes a deficiency of available serotonin. It is inherited as an autosomal recessive trait.
Granulomatous meningoencephalitis (GME) is an inflammatory disease of the central nervous system (CNS) of dogs and, rarely, cats. It is a form of meningoencephalitis. GME is likely second only to encephalitis caused by canine distemper virus as the most common cause of inflammatory disease of the canine CNS. The disease is more common in female dogs of young and middle age. It has a rapid onset. The lesions of GME exist mainly in the white matter of the cerebrum, brainstem, cerebellum, and spinal cord. The cause is only known to be noninfectious and is considered at this time to be idiopathic. Because lesions resemble those seen in allergic meningoencephalitis, GME is thought to have an immune-mediated cause, but it is also thought that the disease may be based on an abnormal response to an infectious agent. One study searched for viral DNA from canine herpesvirus, canine adenovirus, and canine parvovirus in brain tissue from dogs with GME, necrotizing meningoencephalitis, and necrotizing leukoencephalitis, but failed to find any.
Progressive bulbar palsy (PBP) is a medical condition. It belongs to a group of disorders known as motor neuron diseases. PBP is a disease that attacks the nerves supplying the bulbar muscles. These disorders are characterized by the degeneration of motor neurons in the cerebral cortex, spinal cord, brain stem, and pyramidal tracts. This specifically involves the glossopharyngeal nerve (IX), vagus nerve (X), and hypoglossal nerve (XII).

Canine degenerative myelopathy, also known as chronic degenerative radiculomyelopathy, is an incurable, progressive disease of the canine spinal cord that is similar in many ways to amyotrophic lateral sclerosis (ALS). Onset is typically after the age of 7 years and it is seen most frequently in the German shepherd dog, Pembroke Welsh corgi, and boxer dog, though the disorder is strongly associated with a gene mutation in SOD1 that has been found in 43 breeds as of 2008, including the wire fox terrier, Chesapeake Bay retriever, Rhodesian ridgeback, and Cardigan Welsh corgi. Progressive weakness and incoordination of the rear limbs are often the first signs seen in affected dogs, with progression over time to complete paralysis. Myelin is an insulating sheath around neurons in the spinal cord. One proposed cause of degenerative myelopathy is that the immune system attacks this sheath, breaking it down. This results in a loss of communication between nerves in lower body of the animal and the brain.
Guillain–Barré syndrome is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. Typically, both sides of the body are involved, and the initial symptoms are changes in sensation or pain often in the back along with muscle weakness, beginning in the feet and hands, often spreading to the arms and upper body. The symptoms may develop over hours to a few weeks. During the acute phase, the disorder can be life-threatening, with about 15% of people developing weakness of the breathing muscles requiring mechanical ventilation. Some are affected by changes in the function of the autonomic nervous system, which can lead to dangerous abnormalities in heart rate and blood pressure.
Critical illness polyneuropathy (CIP) and critical illness myopathy (CIM) are overlapping syndromes of diffuse, symmetric, flaccid muscle weakness occurring in critically ill patients and involving all extremities and the diaphragm with relative sparing of the cranial nerves. CIP and CIM have similar symptoms and presentations and are often distinguished largely on the basis of specialized electrophysiologic testing or muscle and nerve biopsy. The causes of CIP and CIM are unknown, though they are thought to be a possible neurological manifestation of systemic inflammatory response syndrome. Corticosteroids and neuromuscular blocking agents, which are widely used in intensive care, may contribute to the development of CIP and CIM, as may elevations in blood sugar, which frequently occur in critically ill patients.

Hereditary motor and sensory neuropathies (HMSN) is a name sometimes given to a group of different neuropathies which are all characterized by their impact upon both afferent and efferent neural communication. HMSN are characterised by atypical neural development and degradation of neural tissue. The two common forms of HMSN are either hypertrophic demyelinated nerves or complete atrophy of neural tissue. Hypertrophic condition causes neural stiffness and a demyelination of nerves in the peripheral nervous system, and atrophy causes the breakdown of axons and neural cell bodies. In these disorders, a patient experiences progressive muscle atrophy and sensory neuropathy of the extremities.

Hereditary neuropathy with liability to pressure palsy (HNPP) is a peripheral neuropathy, a condition that affects the nerves. Pressure on the nerves can cause tingling sensations, numbness, pain, weakness, muscle atrophy and even paralysis of the affected area. In normal individuals, these symptoms disappear quickly, but in sufferers of HNPP even a short period of pressure can cause the symptoms to occur. Palsies can last from minutes or days to weeks or even months.
Anti-MAG peripheral neuropathy is a specific type of peripheral neuropathy in which the person's own immune system attacks cells that are specific in maintaining a healthy nervous system. As these cells are destroyed by antibodies, the nerve cells in the surrounding region begin to lose function and create many problems in both sensory and motor function. Specifically, antibodies against myelin-associated glycoprotein (MAG) damage Schwann cells. While the disorder occurs in only 10% of those afflicted with peripheral neuropathy, people afflicted have symptoms such as muscle weakness, sensory problems, and other motor deficits usually starting in the form of a tremor of the hands or trouble walking. There are, however, multiple treatments that range from simple exercises in order to build strength to targeted drug treatments that have been shown to improve function in people with this type of peripheral neuropathy.
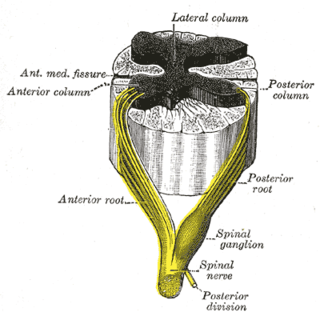
Sensory neuronopathy is a type of peripheral neuropathy that results primarily in sensory symptoms due to destruction of nerve cell bodies in the dorsal root ganglion. The causes of nerve damage are grouped into categories including those due to paraneoplastic causes, immune mediated, infectious, inherited or degenerative causes and those due to toxin exposure. In idiopathic sensory neuronopathy no cause is identified. Idiopathic causes account for about 50% of cases. Sensory neuronopathy differs from the more common length dependent axonal polyneuropathies in that the symptoms do not progress in a distal to proximal pattern, rather symptoms develop in a multifocal, asymmetric, and non-length dependent manner. Ataxia is a prominent symptom early in the disease course. The trigeminal nerve ganglion is also commonly affected leading to facial numbness. Motor nerves are usually not affected however some cases do have mild motor involvement in the form of weakness. Symptoms tend to develop sub-acutely, over weeks, in acquired sensory neuronopathy and more slowly in inherited or primary degenerative cases. In cases of paraneoplastic or infectious sensory neuropathy, treatment is directed at the underlying cancer or infectious cause respectively. Immunomodulatory and anti-inflammatory therapies are also commonly used however their effectiveness is limited.
References
- 1 2 3 4 Chrisman, Cheryl; Clemmons, Roger; Mariani, Christopher; Platt, Simon (2003). Neurology for the Small Animal Practitioner (1st ed.). Teton New Media. ISBN 1-893441-82-2.
- ↑ Braund, K.G. (2003). "Neuropathic Disorders". Braund's Clinical Neurology in Small Animals: Localization, Diagnosis and Treatment. Archived from the original on 8 April 2005. Retrieved 5 September 2006.
- 1 2 3 4 5 6 7 8 9 10 11 12 Ettinger, Stephen J.; Feldman, Edward C. (1995). Textbook of Veterinary Internal Medicine (4th ed.). W.B. Saunders Company. ISBN 0-7216-6795-3.
- ↑ LeCouteur, Richard A. (2003). "Feline Neuromuscular Disorders". Proceedings of the 28th World Congress of the World Small Animal Veterinary Association. Archived from the original on 10 September 2006. Retrieved 5 September 2006.
- ↑ Elad D, Yas-Natan E, Aroch I, Shamir M, Kleinbart S, Hadash D, Chaffer M, Greenberg K, Shlosberg A (2004). "Natural Clostridium botulinum Type C Toxicosis in a Group of Cats". J Clin Microbiol. 42 (11): 5406–8. doi:10.1128/JCM.42.11.5406-5408.2004. PMC 525276 . PMID 15528757.
- ↑ "Botulism". The Merck Veterinary Manual. 2006. Archived from the original on 23 February 2007. Retrieved 10 February 2007.
- 1 2 "Diseases of the Peripheral Nerve and Neuromuscular Junction: Degenerative Diseases". The Merck Veterinary Manual. 2006. Archived from the original on 4 May 2007. Retrieved 10 February 2007.
- ↑ "Diseases of the Peripheral Nerve and Neuromuscular Junction: Metabolic Disorders". The Merck Veterinary Manual. 2006. Archived from the original on 4 May 2007. Retrieved 10 February 2007.
- ↑ Mizisin, Andrew P.; Nelson, RW; Sturges, BK; Vernau, KM; Lecouteur, RA; Williams, DC; Burgers, ML; Shelton, GD (2007). "Comparable myelinated nerve pathology in feline and human diabetes mellitus". Acta Neuropathol. 113 (4): 431–42. doi:10.1007/s00401-006-0163-8. PMID 17237938.
- ↑ "Feline Dysautonomia". The Merck Veterinary Manual. 2006. Retrieved 10 February 2007.
- 1 2 3 "Peripheral Nerve and Muscle Disorders: Small Animals". The Merck Veterinary Manual. 2006. Archived from the original on 2 June 2007. Retrieved 11 February 2007.
- 1 2 "A case study of handling Coonhound Paralysis". 2007. Archived from the original on 16 June 2006. Retrieved 18 February 2007.
- ↑ "Diseases of the Peripheral Nerve and Neuromuscular Junction: Inflammatory Disorders". The Merck Veterinary Manual. 2006. Archived from the original on 26 September 2007. Retrieved 11 December 2007.
- ↑ John C. Fyfe. "Spinal muscular atrophy in Maine Coon Cats (SMA)" (PDF). 2209 Biomedical Physical Sciences, Michigan State University, East Lansing, MI 48824: Laboratory of Comparative Medical Genetics. Archived (PDF) from the original on 21 March 2012. Retrieved 9 March 2011.
{{cite web}}: CS1 maint: location (link) - ↑ Edlow, J. A.; McGillicuddy, D. C (2008). "Tick Paralysis". Infectious Disease Clinics of North America. 22 (3): 397–413. doi:10.1016/j.idc.2008.03.005. PMID 18755381.
- ↑ "Tick Paralysis: Introduction". The Merck Veterinary Manual. 2006. Archived from the original on 23 April 2007. Retrieved 11 February 2007.
- ↑ Chandler, E. A.; et al. (2004) Feline Medicine and Therapeutics. Oxford, UK: Blackwell Pub.; Ames, Iowa: Iowa State Press, pp. 159–160, ISBN 978-1-4051-2814-8.