Immunohistochemistry (IHC) is the most common application of immunostaining. It involves the process of selectively identifying antigens (proteins) in cells of a tissue section by exploiting the principle of antibodies binding specifically to antigens in biological tissues. IHC takes its name from the roots "immuno", in reference to antibodies used in the procedure, and "histo", meaning tissue. Albert Coons conceptualized and first implemented the procedure in 1941.
In clinical trials, a surrogate endpoint is a measure of effect of a specific treatment that may correlate with a real clinical endpoint but does not necessarily have a guaranteed relationship. The National Institutes of Health (USA) defines surrogate endpoint as "a biomarker intended to substitute for a clinical endpoint".

Personalized medicine, precision medicine, or theranostics is a medical model that separates people into different groups—with medical decisions, practices, interventions and/or products being tailored to the individual patient based on their predicted response or risk of disease. The terms personalized medicine, precision medicine, stratified medicine and P4 medicine are used interchangeably to describe this concept though some authors and organisations use these expressions separately to indicate particular nuances.

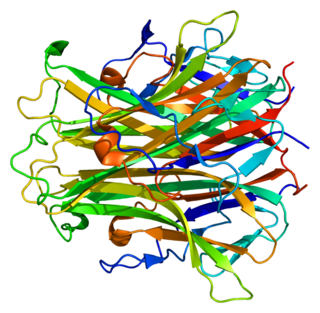
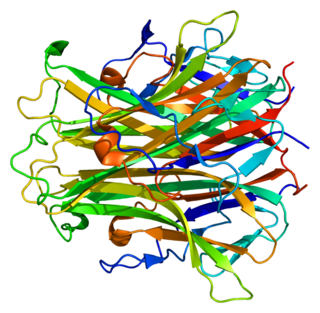
Receptor tyrosine-protein kinase erbB-2, also known as CD340, proto-oncogene Neu, Erbb2 (rodent), or ERBB2 (human), is a protein that in humans is encoded by the ERBB2 gene. ERBB is abbreviated from erythroblastic oncogene B, a gene isolated from avian genome. It is also frequently called HER2 or HER2/neu.
Adjuvant therapy, also known as adjunct therapy, add-on therapy, and adjuvant care, is therapy that is given in addition to the primary or initial therapy to maximize its effectiveness. The surgeries and complex treatment regimens used in cancer therapy have led the term to be used mainly to describe adjuvant cancer treatments. An example of such adjuvant therapy is the additional treatment usually given after surgery where all detectable disease has been removed, but where there remains a statistical risk of relapse due to the presence of undetected disease. If known disease is left behind following surgery, then further treatment is not technically adjuvant. An adjuvant agent modifies the effect of another agent, so adjuvant therapy modifies other therapy.
MammaPrint is a prognostic and predictive diagnostic test for early stage breast cancer patients that assess the risk that a tumor will metastasize to other parts of the body. It gives a binary result, high-risk or low-risk classification, and helps physicians determine whether or not a patient will benefit from chemotherapy. Women with a low risk result can safely forego chemotherapy without decreasing likelihood of disease free survival. MammaPrint is part of the personalized medicine portfolio marketed by Agendia.
Receptor activator of nuclear factor kappa-Β ligand (RANKL), also known as tumor necrosis factor ligand superfamily member 11 (TNFSF11), TNF-related activation-induced cytokine (TRANCE), osteoprotegerin ligand (OPGL), and osteoclast differentiation factor (ODF), is a protein that in humans is encoded by the TNFSF11 gene.

Breast cancer chemotherapy refers to the use of cytotoxic drugs (chemotherapy) in the treatment of breast cancer.
A micrometastasis is a small collection of cancer cells that has been shed from the original tumor and spread to another part of the body through the lymphovascular system. Micrometastases are too few, in size and quantity, to be picked up in a screening or diagnostic test, and therefore cannot be seen with imaging tests such as a mammogram, MRI, ultrasound, PET, or CT scans. These migrant cancer cells may group together to form a second tumor, which is so small that it can only be seen under a microscope. Approximately ninety percent of people who die from cancer die from metastatic disease, since these cells are so challenging to detect. It is important for these cancer cells to be treated immediately after discovery, in order to prevent the relapse and the likely death of the patient.
Breast cancer management takes different approaches depending on physical and biological characteristics of the disease, as well as the age, over-all health and personal preferences of the patient. Treatment types can be classified into local therapy and systemic treatment. Local therapy is most efficacious in early stage breast cancer, while systemic therapy is generally justified in advanced and metastatic disease, or in diseases with specific phenotypes.
Proliferation, as one of the hallmarks and most fundamental biological processes in tumors, is associated with tumor progression, response to therapy, and cancer patient survival. Consequently, the evaluation of a tumor proliferative index has clinical significance in characterizing many solid tumors and hematologic malignancies. This has led investigators to develop different technologies to evaluate the proliferation index in tumor samples. The most commonly used methods in evaluating a proliferative index include mitotic indexing, thymidine-labeling index, bromodeoxyuridine assay, the determination of fraction of cells in various phases of cell cycle, and the immunohistochemical evaluation of cell cycle-associated proteins.
Breast cancer classification divides breast cancer into categories according to different schemes criteria and serving a different purpose. The major categories are the histopathological type, the grade of the tumor, the stage of the tumor, and the expression of proteins and genes. As knowledge of cancer cell biology develops these classifications are updated.
A gene signature or gene expression signature is a single or combined group of genes in a cell with a uniquely characteristic pattern of gene expression that occurs as a result of an altered or unaltered biological process or pathogenic medical condition. This is not to be confused with the concept of gene expression profiling. Activating pathways in a regular physiological process or a physiological response to a stimulus results in a cascade of signal transduction and interactions that elicit altered levels of gene expression, which is classified as the gene signature of that physiological process or response. The clinical applications of gene signatures breakdown into prognostic, diagnostic and predictive signatures. The phenotypes that may theoretically be defined by a gene expression signature range from those that predict the survival or prognosis of an individual with a disease, those that are used to differentiate between different subtypes of a disease, to those that predict activation of a particular pathway. Ideally, gene signatures can be used to select a group of patients for whom a particular treatment will be effective.

Cancer can be treated by surgery, chemotherapy, radiation therapy, hormonal therapy, targeted therapy and synthetic lethality. The choice of therapy depends upon the location and grade of the tumor and the stage of the disease, as well as the general state of the patient. Cancer genome sequencing helps in determining which cancer the patient exactly has for determining the best therapy for the cancer. A number of experimental cancer treatments are also under development. Under current estimates, two in five people will have cancer at some point in their lifetime.
Cancer is a category of disease characterized by uncontrolled cell growth and proliferation. For cancer to develop, genes regulating cell growth and differentiation must be altered; these mutations are then maintained through subsequent cell divisions and are thus present in all cancerous cells. Gene expression profiling is a technique used in molecular biology to query the expression of thousands of genes simultaneously. In the context of cancer, gene expression profiling has been used to more accurately classify tumors. The information derived from gene expression profiling often helps in predicting the patient’s clinical outcome.
DirectHit is a pharmacodiagnostic test used to determine the tumor sensitivity or resistance to drug regimens recommended for the treatment of breast cancer by the National Comprehensive Cancer Network. It is a noninvasive test performed on small amounts of tissue removed during the original surgery lumpectomy, mastectomy, or core biopsy. DirectHit was developed by CCC Diagnostics Inc., a biotechnology company established by former researchers from Johns Hopkins University. DirectHit was launched on 14 January 2010. Currently, it is the only available test for predicting treatment outcomes for anticancer chemotherapy drugs for breast cancer.

A cancer biomarker refers to a substance or process that is indicative of the presence of cancer in the body. A biomarker may be a molecule secreted by a tumor or a specific response of the body to the presence of cancer. Genetic, epigenetic, proteomic, glycomic, and imaging biomarkers can be used for cancer diagnosis, prognosis, and epidemiology. Ideally, such biomarkers can be assayed in non-invasively collected biofluids like blood or serum.
An adaptive clinical trial is a clinical trial that evaluates a medical device or treatment by observing participant outcomes on a prescribed schedule, and modifying parameters of the trial protocol in accord with those observations. The adaptation process generally continues throughout the trial, as prescribed in the trial protocol. Modifications may include dosage, sample size, drug undergoing trial, patient selection criteria and "cocktail" mix. In some cases, trials have become an ongoing process that regularly adds and drops therapies and patient groups as more information is gained. Importantly, the trial protocol is set before the trial begins; the protocol pre-specifies the adaptation schedule and processes.
Kathleen I. Pritchard, is the head of oncology at Sunnybrook Health Sciences Centre in Toronto, Canada, specializing in breast cancer therapies, and leading the clinical trials division of the centre. She has authored numerous studies on women's health, breast cancer, hormone replacement therapy, public health, and research methodology. According to Thomson Reuters, Pritchard was one of the most cited researchers in the world in 2014 and 2015.
Anne Louise Rosenberg is an American surgical oncologist retired from practice in Cherry Hill, New Jersey.