Intrauterine growth restriction (IUGR), or fetal growth restriction, refers to poor growth of a fetus while in the womb during pregnancy. IUGR is defined by clinical features of malnutrition and evidence of reduced growth regardless of an infant's birth weight percentile. The causes of IUGR are broad and may involve maternal, fetal, or placental complications.

Eclampsia is the onset of seizures (convulsions) in a woman with pre-eclampsia. Pre-eclampsia is a hypertensive disorder of pregnancy that presents with three main features: new onset of high blood pressure, large amounts of protein in the urine or other organ dysfunction, and edema. If left untreated, pre-eclampsia can result in long-term consequences for the mother, namely increased risk of cardiovascular diseases and associated complications. In more severe cases, it may be fatal for both the mother and the fetus. The diagnostic criteria for pre-eclampsia is high blood pressure occurring after 20 weeks gestation or during the second half of pregnancy. Most often it occurs during the 3rd trimester of pregnancy and may occur before, during, or after delivery. The seizures are of the tonic–clonic type and typically last about a minute. Following the seizure, there is either a period of confusion or coma. Other complications include aspiration pneumonia, cerebral hemorrhage, kidney failure, pulmonary edema, HELLP syndrome, coagulopathy, placental abruption and cardiac arrest.

Pre-eclampsia is a multi-system disorder specific to pregnancy, characterized by the onset of high blood pressure and often a significant amount of protein in the urine. When it arises, the condition begins after 20 weeks of pregnancy. In severe cases of the disease there may be red blood cell breakdown, a low blood platelet count, impaired liver function, kidney dysfunction, swelling, shortness of breath due to fluid in the lungs, or visual disturbances. Pre-eclampsia increases the risk of undesirable as well as lethal outcomes for both the mother and the fetus including preterm labor. If left untreated, it may result in seizures at which point it is known as eclampsia.

Prenatal testing is a tool that can be used to detect some of these abnormalities at various stages prior to birth. Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of prenatal care that focus on detecting problems with the pregnancy as early as possible. These may be anatomic and physiologic problems with the health of the zygote, embryo, or fetus, either before gestation even starts or as early in gestation as practicable. Screening can detect problems such as neural tube defects, chromosome abnormalities, and gene mutations that would lead to genetic disorders and birth defects, such as spina bifida, cleft palate, Down syndrome, Tay–Sachs disease, sickle cell anemia, thalassemia, cystic fibrosis, muscular dystrophy, and fragile X syndrome. Some tests are designed to discover problems which primarily affect the health of the mother, such as PAPP-A to detect pre-eclampsia or glucose tolerance tests to diagnose gestational diabetes. Screening can also detect anatomical defects such as hydrocephalus, anencephaly, heart defects, and amniotic band syndrome.

Placenta praevia is when the placenta attaches inside the uterus but in a position near or over the cervical opening. Symptoms include vaginal bleeding in the second half of pregnancy. The bleeding is bright red and tends not to be associated with pain. Complications may include placenta accreta, dangerously low blood pressure, or bleeding after delivery. Complications for the baby may include fetal growth restriction.

Gestational hypertension or pregnancy-induced hypertension (PIH) is the development of new hypertension in a pregnant woman after 20 weeks' gestation without the presence of protein in the urine or other signs of pre-eclampsia. Gestational hypertension is defined as having a blood pressure greater than 140/90 on two occasions at least 6 hours apart.
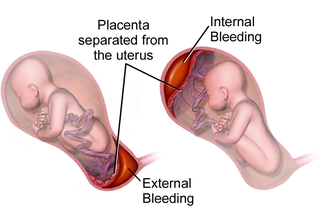
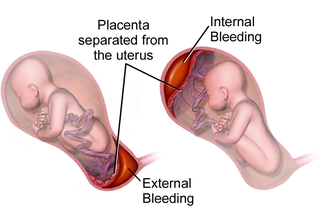
Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.

An abdominal pregnancy is a rare type of ectopic pregnancy where the embryo or fetus is growing and developing outside the womb in the abdomen, but not in the Fallopian tube, ovary or broad ligament.

Intrauterine hypoxia occurs when the fetus is deprived of an adequate supply of oxygen. It may be due to a variety of reasons such as prolapse or occlusion of the umbilical cord, placental infarction, maternal diabetes and maternal smoking. Intrauterine growth restriction may cause or be the result of hypoxia. Intrauterine hypoxia can cause cellular damage that occurs within the central nervous system. This results in an increased mortality rate, including an increased risk of sudden infant death syndrome (SIDS). Oxygen deprivation in the fetus and neonate have been implicated as either a primary or as a contributing risk factor in numerous neurological and neuropsychiatric disorders such as epilepsy, attention deficit hyperactivity disorder, eating disorders and cerebral palsy.
Placental insufficiency or utero-placental insufficiency is the failure of the placenta to deliver sufficient nutrients to the fetus during pregnancy, and is often a result of insufficient blood flow to the placenta. The term is also sometimes used to designate late decelerations of fetal heart rate as measured by cardiotocography or an NST, even if there is no other evidence of reduced blood flow to the placenta, normal uterine blood flow rate being 600mL/min.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.

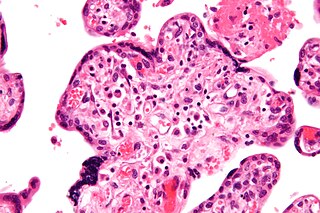
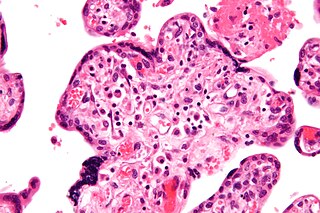
Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.

Prenatal nutrition addresses nutrient recommendations before and during pregnancy. Nutrition and weight management before and during pregnancy has a profound effect on the development of infants. This is a rather critical time for healthy development since infants rely heavily on maternal stores and nutrient for optimal growth and health outcome later in life.
Thyroid disease in pregnancy can affect the health of the mother as well as the child before and after delivery. Thyroid disorders are prevalent in women of child-bearing age and for this reason commonly present as a pre-existing disease in pregnancy, or after childbirth. Uncorrected thyroid dysfunction in pregnancy has adverse effects on fetal and maternal well-being. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Due to an increase in thyroxine binding globulin, an increase in placental type 3 deioidinase and the placental transfer of maternal thyroxine to the fetus, the demand for thyroid hormones is increased during pregnancy. The necessary increase in thyroid hormone production is facilitated by high human chorionic gonadotropin (hCG) concentrations, which bind the TSH receptor and stimulate the maternal thyroid to increase maternal thyroid hormone concentrations by roughly 50%. If the necessary increase in thyroid function cannot be met, this may cause a previously unnoticed (mild) thyroid disorder to worsen and become evident as gestational thyroid disease. Currently, there is not enough evidence to suggest that screening for thyroid dysfunction is beneficial, especially since treatment thyroid hormone supplementation may come with a risk of overtreatment. After women give birth, about 5% develop postpartum thyroiditis which can occur up to nine months afterwards. This is characterized by a short period of hyperthyroidism followed by a period of hypothyroidism; 20–40% remain permanently hypothyroid.

A high-risk pregnancy is one where the mother or the fetus has an increased risk of adverse outcomes compared to uncomplicated pregnancies. No concrete guidelines currently exist for distinguishing “high-risk” pregnancies from “low-risk” pregnancies; however, there are certain studied conditions that have been shown to put the mother or fetus at a higher risk of poor outcomes. These conditions can be classified into three main categories: health problems in the mother that occur before she becomes pregnant, health problems in the mother that occur during pregnancy, and certain health conditions with the fetus.
A pre-existing disease in pregnancy is a disease that is not directly caused by the pregnancy, in contrast to various complications of pregnancy, but which may become worse or be a potential risk to the pregnancy. A major component of this risk can result from necessary use of drugs in pregnancy to manage the disease.
The anomaly scan, also sometimes called the anatomy scan, 20-week ultrasound, or level 2 ultrasound, evaluates anatomic structures of the fetus, placenta, and maternal pelvic organs. This scan is an important and common component of routine prenatal care. The function of the ultrasound is to measure the fetus so that growth abnormalities can be recognized quickly later in pregnancy, to assess for congenital malformations and multiple pregnancies, and to plan method of delivery.

Lesley Margaret Elizabeth McCowan is a New Zealand medical researcher and academic specialising in maternal health. She is currently a full professor and head of obstetrics and gynaecology at the University of Auckland.
Fetal programming, also known as prenatal programming, is the theory that environmental cues experienced during fetal development play a seminal role in determining health trajectories across the lifespan.