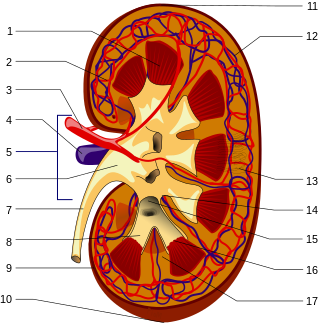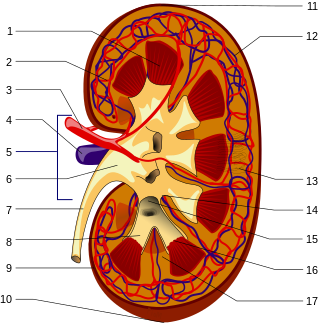
Nephrology is a specialty for both adult internal medicine and pediatric medicine that concerns the study of the kidneys, specifically normal kidney function and kidney disease, the preservation of kidney health, and the treatment of kidney disease, from diet and medication to renal replacement therapy. The word "renal" is an adjective meaning "relating to the kidneys", and its roots are French or late Latin. Whereas according to some opinions, "renal" and "nephro" should be replaced with "kidney" in scientific writings such as "kidney medicine" or "kidney replacement therapy", other experts have advocated preserving the use of renal and nephro as appropriate including in "nephrology" and "renal replacement therapy", respectively.

Henoch–Schönlein purpura (HSP), also known as IgA vasculitis, is a disease of the skin, mucous membranes, and sometimes other organs that most commonly affects children. In the skin, the disease causes palpable purpura, often with joint pain and abdominal pain. With kidney involvement, there may be a loss of small amounts of blood and protein in the urine, but this usually goes unnoticed; in a small proportion of cases, the kidney involvement proceeds to chronic kidney disease. HSP is often preceded by an infection, such as a throat infection.
Glomerulonephritis (GN) is a term used to refer to several kidney diseases. Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the name, but not all diseases necessarily have an inflammatory component.

Membranous glomerulonephritis (MGN) is a slowly progressive disease of the kidney affecting mostly people between ages of 30 and 50 years, usually white people.

Minimal change disease is a disease affecting the kidneys which causes nephrotic syndrome. Nephrotic syndrome leads to the loss of significant amounts of protein in the urine, which causes the widespread edema and impaired kidney function commonly experienced by those affected by the disease. It is most common in children and has a peak incidence at 2 to 6 years of age. MCD is responsible for 10–25% of nephrotic syndrome cases in adults. It is also the most common cause of nephrotic syndrome of unclear cause (idiopathic) in children.

Nephritic syndrome is a syndrome comprising signs of nephritis, which is kidney disease involving inflammation. It often occurs in the glomerulus, where it is called glomerulonephritis. Glomerulonephritis is characterized by inflammation and thinning of the glomerular basement membrane and the occurrence of small pores in the podocytes of the glomerulus. These pores become large enough to permit both proteins and red blood cells to pass into the urine. By contrast, nephrotic syndrome is characterized by proteinuria and a constellation of other symptoms that specifically do not include hematuria. Nephritic syndrome, like nephrotic syndrome, may involve low level of albumin in the blood due to the protein albumin moving from the blood to the urine.
Renal osteodystrophy is currently defined as an alteration of bone morphology in patients with chronic kidney disease (CKD). It is one measure of the skeletal component of the systemic disorder of chronic kidney disease-mineral and bone disorder (CKD-MBD). The term "renal osteodystrophy" was coined in 1943, 60 years after an association was identified between bone disease and kidney failure.

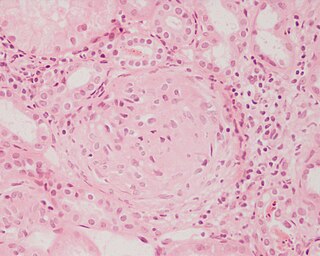
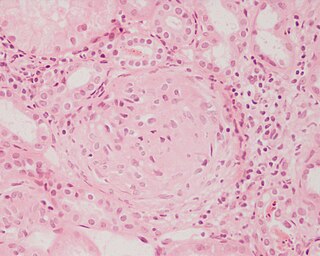
Acute proliferative glomerulonephritis is a disorder of the small blood vessels of the kidney. It is a common complication of bacterial infections, typically skin infection by Streptococcus bacteria types 12, 4 and 1 (impetigo) but also after streptococcal pharyngitis, for which it is also known as postinfectious glomerulonephritis (PIGN) or poststreptococcal glomerulonephritis (PSGN). It can be a risk factor for future albuminuria. In adults, the signs and symptoms of infection may still be present at the time when the kidney problems develop, and the terms infection-related glomerulonephritis or bacterial infection-related glomerulonephritis are also used. Acute glomerulonephritis resulted in 19,000 deaths in 2013, down from 24,000 deaths in 1990 worldwide.

Mesangial proliferative glomerulonephritis (MesPGN) is a morphological pattern characterized by a numerical increase in mesangial cells and expansion of the extracellular matrix within the mesangium of the glomerulus. The increase in the number of mesangial cells can be diffuse or local and immunoglobulin and/or complement deposition can also occur. MesPGN is associated with a variety of disease processes affecting the glomerulus, though can be idiopathic. The clinical presentation of MesPGN usually consists of hematuria or nephrotic syndrome. Treatment is often consistent with the histologic pattern of and/or disease process contributing to mesangial proliferative glomerulonephritis, and usually involves some form of immunosuppressant.
Amin J. Barakat is a Lebanese-American physician known for the diagnosis Barakat syndrome.

Renal biopsy is a medical procedure in which a small piece of kidney is removed from the body for examination, usually under a microscope. Microscopic examination of the tissue can provide information needed to diagnose, monitor or treat problems of the kidney.
Renal cortical necrosis (RCN) is a rare cause of acute kidney failure. The condition is "usually caused by significantly diminished arterial perfusion of the kidneys due to spasms of the feeding arteries, microvascular injury, or disseminated intravascular coagulation" and is the pathological progression of acute tubular necrosis. It is frequently associated with obstetric catastrophes such as abruptio placentae and septic shock, and is three times more common in developing nations versus industrialized nations.
Douglas Montagu Temple Gairdner FRCP was a Scottish paediatrician, research scientist, academic and author. Gairdner was principally known for a number of research studies in neonatology at a time when that subject was being developed as perhaps the most rewarding application of basic physiology to patient care, and later his most important contributions as editor, firstly editing Recent Advances in Paediatrics, and then of Archives of Disease in Childhood for 15 years, turning the latter into an international journal of repute with its exemplary standards of content and presentation.
Jochen H.H. Ehrich is a German pediatric doctor in the fields of nephrology and tropical medicine, professor emeritus and Former Head of the Department of Paediatric Kidney, Liver and Metabolic Diseases at the Children’s Hospital, Hannover Medical School, in Hannover, Germany.

Otto Herbert Wolff, was a German born medical scientist, paediatrician and was the Nuffield Professor of Child Health at Great Ormond Street Hospital. Wolff was notable for being one of the first paediatricians in Britain to set up a clinic for obese children. Later research into plasma lipids with Harold Salt pioneered the techniques of lipoprotein electrophoresis. He later conducted research into the role of lipid disturbance in childhood as a precursor of coronary artery disease and his recognition in 1960 of the rare condition of abetalipoproteinaemia. Wolff was also co-discoverer of the Edwards syndrome in abnormal chromosomes.

Thomas Martin Barratt was a British paediatrician and professor of paediatric nephrology. Barratt was most notable for developing a specialist service for children with kidney diseases in Britain, bringing peritoneal dialysis, haemodialysis, and later renal transplantation to ever younger children. Barratt was an early advocate for multidisciplinary care and developed a model that was later taken up by many other specialist centres across the world. His research led to a new treatments for many types of childhood kidney diseases., and for research into childhood Nephrotic syndrome and Hemolytic-uremic syndrome.
John Farrar Soothill was an English medical doctor. He began his career as a nephrologist and later became a paediatric immunologist at Great Ormond Street Hospital.
Gavin Cranston Arneil was a Scottish paediatric nephrologist. At the Royal Hospital for Sick Children in Glasgow, he established the first specialised unit in Britain for children with kidney disease.

The International Pediatric Nephrology Association (IPNA) is an association to promote the knowledge and communication among the pediatric nephrologists and improve the diagnosis, treatment and prevention of kidney disease at children around the world. IPNA has 1600 members representing 103 countries.
Friedhelm Hildebrandt is the William E. Harmon Professor of Pediatrics at Harvard Medical School and Chief of the Division of Nephrology at Boston Children's Hospital. He was formerly an Investigator of the Howard Hughes Medical Institute (HHMI) and the Frederick G.L. Huetwell Professor of Pediatrics at the University of Michigan.