Related Research Articles

June Kathleen Lloyd, Baroness Lloyd of Highbury was a British paediatrician and, in retirement, a cross bench member of the House of Lords. June Lloyd was a determined advocate for children's health and was instrumental in the establishment of the Royal College of Paediatrics and Child Health. In 1996, the college gained its royal status. She was also known for discovering that the damage caused to patients by the rare metabolic disease oQ-betalipoproteinaemia, that could be avoided by the use of Vitamin E. She was also known for discovering the role of lipid metabolism in health and disease in childhood, which was original and difficult to investigate at that time.
The Royal College of Paediatrics and Child Health, often referred to as the RCPCH, is the professional body for paediatricians in the United Kingdom. It is responsible for the postgraduate training of paediatricians and conducts the Membership of the Royal College of Paediatrics and Child Health (MRCPCH) exams. It also awards the Diploma in Child Health (DCH), which is taken by many doctors who plan a career in general practice. Members of the college use the postnominal initials 'MRCPCH' while Fellows use 'FRCPCH'.
Sir James Calvert Spence, & Bar was an English paediatrician who was a pioneer in the field of social paediatrics. He was a founding member of the British Paediatric Association.
Sir John Peter Mills Tizard was a British paediatrician and professor at the University of Oxford. Tizard was principally notable for important research into neonatology and paediatric neurology and being a founder member of the Neonatal Society in 1959. Tizard was considered the most distinguished academic children's physician of his generation.

The UCL Great Ormond Street Institute of Child Health (ICH) is an academic department of the Faculty of Population Health Sciences of University College London (UCL) and is located in London, United Kingdom. It was founded in 1946 and together with its clinical partner Great Ormond Street Hospital (GOSH), forms the largest concentration of children's health research in Europe. In 1996 the Institute merged with University College London. Current research focusses on broad biomedical topics within child health, ranging from developmental biology, to genetics, to immunology and epidemiology.
Victor Dubowitz is a British neurologist and professor emeritus at Imperial College London. He is principally known along with his wife Lilly Dubowitz for developing two clinical tests, the Dubowitz Score to estimate gestational age and the other for the systematic neurological examination of the newborn.

John Oldroyd Forfar, MC, FRSE was a Scottish paediatrician and academic. He served in the Royal Army Medical Corps during the Second World War and later became a leading civilian paediatrician. He was Professor of Child Life and Health at the University of Edinburgh from 1964 to 1982. He was President of the British Paediatric Association from 1985 to 1988, and was instrumental in the founding of the Royal College of Paediatrics and Child Health.
Sir Terence John Stephenson, is a Northern Irish consultant paediatric doctor and chair of the Health Research Authority (HRA). He is also the Nuffield Professor of Child Health at University College London (UCL). Stephenson was most notable for guiding the RCPCH in agreeing 10 published national standards, Facing the Future: Standards for Paediatric Services. This was the first time the College committed publicly to a defined set of standards for all children receiving inpatient care or assessment across the UK.
Sir (Charles) Eric Stroud was a Welsh-born British paediatrician and Professor of Child Health, King's College School of Medicine and Dentistry.

Hilary Dawn Cass, Baroness Cass,, is a British paediatrician. She was the chair of the British Academy of Childhood Disability, established the Rett Clinic for children with Rett syndrome, and has worked to develop palliative care for children. She led the Cass Review of gender identity services in England, which was completed in 2024. Cass was appointed to the House of Lords as a crossbench life peer in the same year.
Sir David Hull was a British paediatrician. Hull was most notable for research and for a paper he published in 1963 in the Journal of Physiology with Michael Dawkins, about research into brown fat, an adipose-like tissue found in hibernating animals and in the human Infant and for later contributions considered outstanding in research conducted on Lipid metabolism and Thermoregulation.
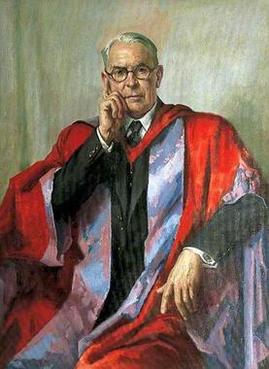
Sir Alan Aird Moncrieff, was a British paediatrician and professor emeritus at University of London. He was most notable for developing the first premature-baby unit in 1947. It was Moncrief who recognised and developed the concept of daily parental visits to the ward, which he developed while at Great Ormond Street, well before the need for this became recognised, and with his ward sister, published an article on Hospital Visiting for Children in 1949.

Ronald Charles MacKeith FRCP was a British paediatrician. MacKeith was prolific in his endeavours. He was principally known for establishing the first cerebral palsy advice clinic, which was to become in 1964, the larger and more comprehensive Newcomen Centre for disabled children in Guy's Hospital. He founded the British Paediatric Neurology Association and the medical journal, Developmental Medicine & Child Neurology. His work gained recognition of the field of paediatric neurology as a science in several European countries.

Seymour Donald Mayneord Court was a British paediatrician who was known for his achievements in the fields of respiratory disease and the epidemiology of disease in childhood. He was also known for working, in a primary role, that established the importance of research into the social and behavioural aspects of illness in childhood.

Neil Simson Gordon was a Scottish paediatric neurologist, who conducted research into eponymic diseases including chronic handicaps, cerebral palsy, epilepsy, disorders of languages and learning disabilities. Gordon was one of the first to initiate comprehensive multidisciplinary assessment centres for children. He has been described as the "wise grand old man of UK paediatric neurology" and first specialist paediatric neurologist to be appointed outside London.
Lewis Spitz is a paediatric surgeon who is internationally recognised as a leader in paediatric surgery and is known for his work on congenital abnormalities of the oesophagus, particularly oesophageal atresia, oesophageal replacement and gastroesophageal reflux especially in neurologically impaired children. He championed the plight of children with cerebral palsy and other congenital disorders; demonstrating that appropriate surgery could improve their quality of life. He is the leading authority in the management of conjoined twins and is recognised as the foremost international expert in this field. Spitz is the Emeritus Nuffield Professor of Paediatric Surgery.

British Association of Perinatal Medicine, known as BAPM, is a charitable organization that was founded in Bristol in 1976 that is most notable for being a pressure group to advance the standards of perinatal care within the United Kingdom by a dedicated core of professional physicians who are accredited by examination.
Elizabeth Jane Elliott is an Australian clinician scientist. She is a Member of the Order of Australia (AM), for services to paediatrics and child health, as well as an Elected Fellow of the Australian Academy of Health and Medical Science (AAHMS), Fellow of the Royal Society of NSW, and Fellow of the Academy of Child and Adolescent Health. She was the first female to win the James Cook Medal, awarded by the Royal Society of NSW for contributions to human welfare. She is a Distinguished Professor of paediatrics at the University of Sydney and a Consultant Paediatrician at the Sydney Children’s Hospitals Network, Westmead, and regarded as a "pioneer in fetal alcohol spectrum disorder, advocacy and patient care".
John Kingdon Guy Webb was an English paediatrician and first-class cricketer. After attending the University of Oxford, where he played first-class cricket, Webb became a paediatrician who spent eighteen years at the Christian Medical College in Vellore, Tamil Nadu and was instrumental in helping set up a paediatric medical structure in the country.
Abdul Rashid Gatrad (1946-) is a Malawi-born consultant paediatrician of Memon heritage, working in England.
References
- 1 2 Mosley, Charles, ed. (2003). Burke's Peerage, Baronetage & Knighthood (107 ed.). Burke's Peerage & Gentry. p. 1731. ISBN 0-9711966-2-1.
- 1 2 3 4 5 6 7 8 9 10 11 12 "Professor Sir David Hall". The Royal College of Paediatrics and Child Health. The Royal College of Paediatrics and Child Health. 28 February 2017. Retrieved 22 November 2018.
- 1 2 3 4 5 "Professor, Sir David Hall". Honorary award holders. Anglia Ruskin University. Retrieved 22 November 2018.
- 1 2 "The "Family - Nurse Partnership": developing an instrument for identification, assessment and recruitment of clients" (pdf). Digital Education Resource Archive. Disclaimer: University of College, Institute of Education. October 2007. Retrieved 23 November 2018.
- ↑ "Research Report DFE-RR068" (PDF). BirbeckUniversity of London. Department of Education. Retrieved 25 November 2018.
- 1 2 Sample, Ian (27 June 2006). "Draw line under MMR scare, plead top doctors". Guardian News and Media Limited. The Guardian. Retrieved 25 November 2018.
- ↑ Oberklaid, F.; Baird, G.; Blair, M.; Melhuish, E.; Hall, D. (22 August 2013). "Children's health and development: approaches to early identification and intervention". Archives of Disease in Childhood. 98 (12): 1008–1011. doi:10.1136/archdischild-2013-304091.
- ↑ Hall, David M B (1992). Hall, David (ed.). Health for all children: a programme for child health surveillance: the report of the Joint Working Party on Child Health Surveillance (xix, 181 p. : ill, pdf). Oxford medical publications (2nd ed.). Oxford, New York: Oxford University Press. ISBN 9780192621139. LCCN 91-28844.
- ↑ Alan Craft; Keith Dodd (21 March 2017). From an Association to a Royal College: The History of the British Paediatric Association and Royal College of Paediatrics and Child Health 1988-2016. Springer. p. 226. ISBN 978-3-319-43582-4 . Retrieved 22 November 2018.
- 1 2 3 4 5 David M B Hall; David Elliman (7 September 2006). Health for All Children: Revised Fourth Edition. OUP Oxford. p. 3. ISBN 978-0-19-857084-4 . Retrieved 24 November 2018.
- ↑ Hall, David M B; Williams, Jonathan; Elliman, David (2009). The child surveillance handbook (3 ed.). Oxford, New York: Radcliffe Publishing. ISBN 9781846191091. OCLC 271774331.