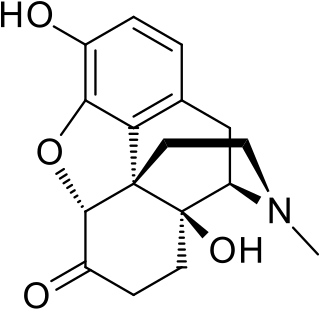
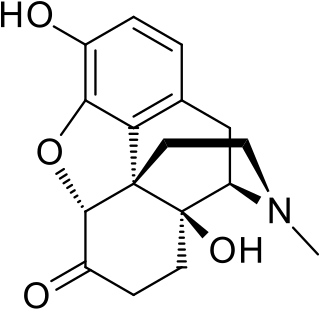
Heroin, also known as diacetylmorphine and diamorphine among other names, is a morphinan opioid substance derived from the dried latex of the Papaver somniferum plant and is mainly used as a recreational drug for its euphoric effects. Medical-grade diamorphine is used as a pure hydrochloride salt. Various white and brown powders sold illegally around the world as heroin are routinely diluted with cutting agents. Black tar heroin is a variable admixture of morphine derivatives—predominantly 6-MAM (6-monoacetylmorphine), which is the result of crude acetylation during clandestine production of street heroin. Heroin is used medically in several countries to relieve pain, such as during childbirth or a heart attack, as well as in opioid replacement therapy.

Botulism is a rare and potentially fatal illness caused by a toxin produced by the bacterium Clostridium botulinum. The disease begins with weakness, blurred vision, feeling tired, and trouble speaking. This may then be followed by weakness of the arms, chest muscles, and legs. Vomiting, swelling of the abdomen, and diarrhea may also occur. The disease does not usually affect consciousness or cause a fever.

Harm reduction, or harm minimization, refers to a range of intentional practices and public health policies designed to lessen the negative social and/or physical consequences associated with various human behaviors, both legal and illegal. Harm reduction is used to decrease negative consequences of recreational drug use and sexual activity without requiring abstinence, recognizing that those unable or unwilling to stop can still make positive change to protect themselves and others.
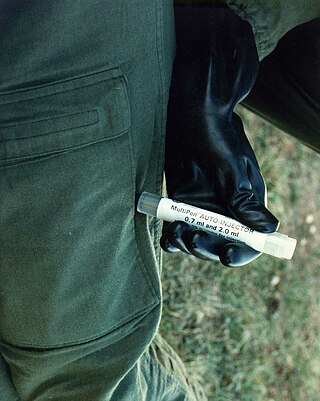
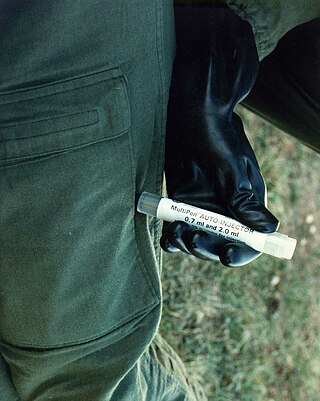
An autoinjector is a medical device designed to deliver a dose of a particular drug. The injectors were initially designed to overcome the hesitation associated with self-administration of the needle-based drug delivery device.

In pharmacology and toxicology, a route of administration is the way by which a drug, fluid, poison, or other substance is taken into the body.

Subcutaneous administration is the insertion of medications beneath the skin either by injection or infusion.

Intramuscular injection, often abbreviated IM, is the injection of a substance into a muscle. In medicine, it is one of several methods for parenteral administration of medications. Intramuscular injection may be preferred because muscles have larger and more numerous blood vessels than subcutaneous tissue, leading to faster absorption than subcutaneous or intradermal injections. Medication administered via intramuscular injection is not subject to the first-pass metabolism effect which affects oral medications.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

An injection is the act of administering a liquid, especially a drug, into a person's body using a needle and a syringe. An injection is considered a form of parenteral drug administration; it does not involve absorption in the digestive tract. This allows the medication to be absorbed more rapidly and avoid the first pass effect. There are many types of injection, which are generally named after the body tissue the injection is administered into. This includes common injections such as subcutaneous, intramuscular, and intravenous injections, as well as less common injections such as intraperitoneal, intraosseous, intracardiac, intraarticular, and intracavernous injections.

Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, it is typically started when withdrawal symptoms have begun and for the first two days of treatment under direct observation of a health-care provider.
Oxymorphone is a highly potent opioid analgesic indicated for treatment of severe pain. Pain relief after injection begins after about 5–10 minutes, after oral administration it begins after about 30 minutes, and lasts about 3–4 hours for immediate-release tablets and 12 hours for extended-release tablets. The elimination half-life of oxymorphone is much faster intravenously, and as such, the drug is most commonly used orally. Like oxycodone, which metabolizes to oxymorphone, oxymorphone has a high potential to be abused.

Xylazine is a drug used for sedation, anesthesia, muscle relaxation, and analgesia in animals such as horses, cattle, and other non-human mammals. It is an analog of clonidine and an agonist at the α2 class of adrenergic receptor.

Black tar heroin, also known as black dragon, is a form of heroin that is sticky like tar or hard like coal. Its dark color is the result of crude processing methods that leave behind impurities. Despite its name, black tar heroin can also be dark orange or dark brown in appearance.

Drug injection is a method of introducing a drug into the bloodstream via a hollow hypodermic needle, which is pierced through the skin into the body. Intravenous therapy, a form of drug injection, is universally practiced in modernized medical care. As of 2004, there were 13.2 million people worldwide who self-administered injection drugs outside of medical supervision, of which 22% are from developed countries.

An opioid overdose is toxicity due to excessive consumption of opioids, such as morphine, codeine, heroin, fentanyl, tramadol, and methadone. This preventable pathology can be fatal if it leads to respiratory depression, a lethal condition that can cause hypoxia from slow and shallow breathing. Other symptoms include small pupils, and unconsciousness, however its onset can depend on the method of ingestion, the dosage and individual risk factors. Although there were over 110,000 deaths in 2017 due to opioids, individuals who survived also faced adverse complications, including permanent brain damage.
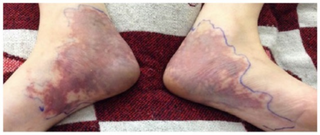
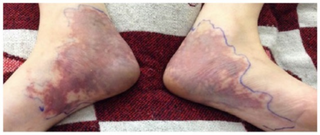
Livedoid dermatitis is a iatrogenic cutaneous reaction that occurs immediately after a drug injection. It presents as an immediate, extreme pain around the injection site, with overlying skin rapidly becoming erythematous, violaceous, or blanched and sometimes with reticular pattern. The reaction eventually leads to variable degrees of necrosis to the skin and underlying tissue. The wound eventually heals, but can lead to atrophic, disfiguring scarring.

Intradermal injection is a shallow or superficial injection of a substance into the dermis, which is located between the epidermis and the hypodermis. For certain substances, administration via an ID route can result in a faster systemic uptake compared with subcutaneous injections, leading to a stronger immune response to vaccinations, immunology and novel cancer treatments, and faster drug uptake. Additionally, since administration is closer to the surface of the skin, the body's reaction to substances is more easily visible. However, due to complexity of the procedure compared to subcutaneous injection and intramuscular injection, administration via ID is relatively rare, and is only used for tuberculosis and allergy tests, Monkeypox vaccination, and certain therapies.

In the United States, the opioid epidemic is an extensive ongoing overuse of opioid medications, both from medical prescriptions and illegal sources. The epidemic began in the United States in the late 1990s, according to the Centers for Disease Control and Prevention (CDC), when opioids were increasingly prescribed for pain management, resulting in a rise in overall opioid use throughout subsequent years. The great majority of Americans who use prescription opioids do not believe that they are misusing them.

An injector pen is a device used for injecting medication under the skin. First introduced in the 1980s, injector pens are designed to make injectable medication easier and more convenient to use, thus increasing patient adherence. The primary difference between injector pens and traditional vial and syringe administration is the easier use of an injector pen by people with low dexterity, poor vision, or who need portability to administer medicine on time. Injector pens also decrease the fear or adversity towards self-injection of medications, which increases the likelihood that a person takes the medication.

A depot injection is a term for an injection formulation of a medication which releases slowly over time to permit less frequent administration of a medication. They are designed to increase medication adherence and consistency, especially in patients who commonly forget to take their medicine. Depot injections can be created by modifying the drug molecule itself, as in the case of prodrugs, or by modifying the way it is administered, as in the case of oil/lipid suspensions. Depot injections can have a duration of action of one month or greater and are available for many types of drugs, including antipsychotics and hormones.