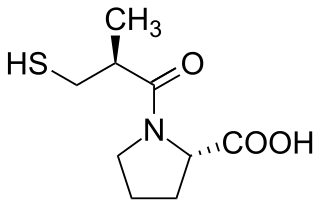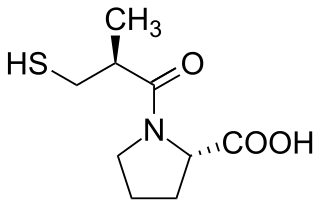
Angiotensin-converting-enzyme inhibitors are a class of medication used primarily for the treatment of high blood pressure and heart failure. This class of medicine works by causing relaxation of blood vessels as well as a decrease in blood volume, which leads to lower blood pressure and decreased oxygen demand from the heart.

Dorothy Mary Crowfoot Hodgkin was a Nobel Prize-winning English chemist who advanced the technique of X-ray crystallography to determine the structure of biomolecules, which became essential for structural biology.

The renin-angiotensin system (RAS), or renin-angiotensin-aldosterone system (RAAS), is a hormone system that regulates blood pressure, fluid, and electrolyte balance, and systemic vascular resistance.

Angiotensin is a peptide hormone that causes vasoconstriction and an increase in blood pressure. It is part of the renin–angiotensin system, which regulates blood pressure. Angiotensin also stimulates the release of aldosterone from the adrenal cortex to promote sodium retention by the kidneys.
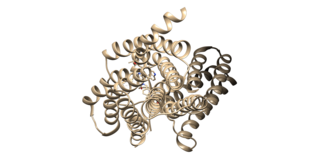
The angiotensin II receptors, (ATR1) and (ATR2), are a class of G protein-coupled receptors with angiotensin II as their ligands. They are important in the renin–angiotensin system: they are responsible for the signal transduction of the vasoconstricting stimulus of the main effector hormone, angiotensin II.
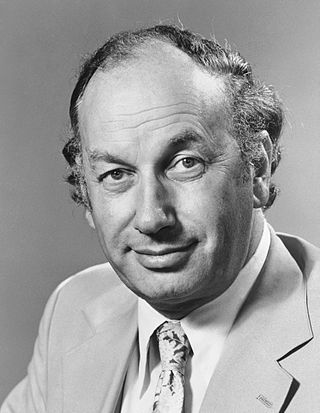
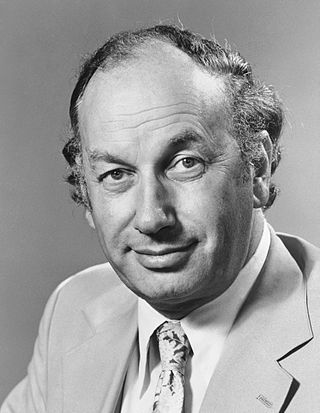
Sir John Robert Vane was a British pharmacologist who was instrumental in the understanding of how aspirin produces pain-relief and anti-inflammatory effects and his work led to new treatments for heart and blood vessel disease and introduction of ACE inhibitors. He was awarded the Nobel Prize in Physiology or Medicine in 1982 along with Sune Bergström and Bengt Samuelsson for "their discoveries concerning prostaglandins and related biologically active substances".

Renal artery stenosis (RAS) is the narrowing of one or both of the renal arteries, most often caused by atherosclerosis or fibromuscular dysplasia. This narrowing of the renal artery can impede blood flow to the target kidney, resulting in renovascular hypertension – a secondary type of high blood pressure. Possible complications of renal artery stenosis are chronic kidney disease and coronary artery disease.

Sir Walter Fred Bodmer is a German-born British human geneticist.

Renovascular hypertension is a condition in which high blood pressure is caused by the kidneys' hormonal response to narrowing of the arteries supplying the kidneys. When functioning properly this hormonal axis regulates blood pressure. Due to low local blood flow, the kidneys mistakenly increase blood pressure of the entire circulatory system. It is a form of secondary hypertension - a form of hypertension whose cause is identifiable.

Dame Alice Josephine Mary Taylor Barnes,, known professionally as Dr Josephine Barnes, was a leading English obstetrician and gynaecologist. She was the first female president of the British Medical Association, 1979. Barnes was active in the Women's National Cancer Control Campaign with cancer screening.

Dame Bridget Margaret Ogilvie, is an Australian and British scientist.
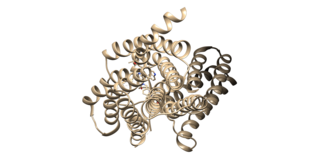
Angiotensin II receptor type 1(AT1) is a Gq/11-coupled G protein-coupled receptor (GPCR) and the best characterized angiotensin receptor. It is encoded in humans by the AGTR1 gene. AT1 has vasopressor effects and regulates aldosterone secretion. It is an important effector controlling blood pressure and volume in the cardiovascular system. Angiotensin II receptor blockers are drugs indicated for hypertension, diabetic nephropathy and congestive heart failure.

Brigitte Alice Askonas was a British immunologist and a visiting professor at Imperial College London from 1995.
Max Leonard Rosenheim, Baron Rosenheim, KBE, PRCP, FRS was a British physician and academic.
Jeremiah Noah Morris was a Scottish epidemiologist who established the importance of physical activity in preventing cardiovascular disease.

Glomerular hyperfiltration is a situation where the filtration elements in the kidneys called glomeruli produce excessive amounts of pro-urine. It can be part of a number of medical conditions particularly diabetic nephropathy.
Aileen Kirkpatrick Adams is a British retired consultant anaesthetist. She turned 100 in September 2023.

Pierre Corvol is a French doctor and biology researcher. He was director of the Collège de France from 2006 to August 2012.
Page kidney or Page phenomena is a potentially reversible form of secondary arterial hypertension caused by external compression of the renal parenchyma by some perirenal process. Any process that causes mass effect can be a potential cause of Page kidney. Hematomas, urinomas, tumors, cysts, lymphoceles, and aneurysms have all been reported in the literature. The compression is believed to cause activation of the renin–angiotensin–aldosterone system (RAAS) via microvascular ischemia.