Related Research Articles

The human immunodeficiency viruses (HIV) are two species of Lentivirus that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immune system allows life-threatening opportunistic infections and cancers to thrive. Without treatment, average survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype. In most cases, HIV is a sexually transmitted infection and occurs by contact with or transfer of blood, pre-ejaculate, semen, and vaginal fluids. Research has shown that HIV is untransmittable through condomless sexual intercourse if the HIV-positive partner has a consistently undetectable viral load. Non-sexual transmission can occur from an infected mother to her infant during pregnancy, during childbirth by exposure to her blood or vaginal fluid, and through breast milk. Within these bodily fluids, HIV is present as both free virus particles and virus within infected immune cells.

Antiviral drugs are a class of medication used for treating viral infections. Most antivirals target specific viruses, while a broad-spectrum antiviral is effective against a wide range of viruses. Unlike most antibiotics, antiviral drugs do not destroy their target pathogen; instead they inhibit its development.

Hepatitis C is an infectious disease caused by the hepatitis C virus (HCV) that primarily affects the liver; it is a type of viral hepatitis. During the initial infection people often have mild or no symptoms. Occasionally a fever, dark urine, abdominal pain, and yellow tinged skin occurs. The virus persists in the liver in about 75% to 85% of those initially infected. Early on chronic infection typically has no symptoms. Over many years however, it often leads to liver disease and occasionally cirrhosis. In some cases, those with cirrhosis will develop serious complications such as liver failure, liver cancer, or dilated blood vessels in the esophagus and stomach.
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs in an attempt to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same sex and opposite sex partners so long as the HIV-positive partner maintains an undetectable viral load.
Viral hepatitis is liver inflammation due to a viral infection. It may present in acute form as a recent infection with relatively rapid onset, or in chronic form.
Following infection with HIV-1, the rate of clinical disease progression varies between individuals. Factors such as host susceptibility, genetics and immune function, health care and co-infections as well as viral genetic variability may affect the rate of progression to the point of needing to take medication in order not to develop AIDS.
Human Immunodeficiency Virus (HIV) and Hepatitis C Virus (HCV) co-infection is a multi-faceted, chronic condition that significantly impacts public health. According to the World Health Organization (WHO), 2 to 15% of those infected with HIV are also affected by HCV, increasing their risk of morbidity and mortality due to accelerated liver disease. The burden of co-infection is especially high in certain high-risk groups, such as intravenous drug users and men who have sex with men. These individuals who are HIV-positive are commonly co-infected with HCV due to shared routes of transmission including, but not limited to, exposure to HIV-positive blood, sexual intercourse, and passage of the Hepatitis C virus from mother to infant during childbirth.
HIV superinfection is a condition in which a person with an established human immunodeficiency virus infection acquires a second strain of HIV, often of a different subtype. These can form a recombinant strain that co-exists with the strain from the initial infection, as well from reinfection with a new virus strain, and may cause more rapid disease progression or carry multiple resistances to certain HIV medications.
Long-term nonprogressors (LTNPs), sometimes also called elite controllers, are individuals infected with HIV, who maintain a CD4 count greater than 500 without antiretroviral therapy with a detectable viral load. Many of these patients have been HIV positive for 30 years without progressing to the point of needing to take medication in order not to develop AIDS. They have been the subject of a great deal of research, since an understanding of their ability to control HIV infection may lead to the development of immune therapies or a therapeutic vaccine. The classification "Long-term non-progressor" is not permanent, because some patients in this category have gone on to develop AIDS.

Janice Ellen Clements is Vice Dean for Faculty at the Johns Hopkins School of Medicine and the Mary Wallace Stanton Professor of Faculty Affairs. She is a professor in the departments of Molecular and Comparative Pathobiology, Neurology, and Pathology, and has a joint appointment in molecular biology and genetics. Her molecular biology and virology research examines lentiviruses and how they cause neurological diseases.
AntiViral-HyperActivation Limiting Therapeutics (AV-HALTs) are an investigational class of antiretroviral drugs used to treat Human Immunodeficiency Virus (HIV) infection. Unlike other antiretroviral agents given to reduce viral replication, AV-HALTs are single or combination drugs designed to reduce the rate of viral replication while, at the same time, also directly reducing the state of immune system hyperactivation now believed to drive the loss of CD4+ T helper cells leading to disease progression and Acquired Immunodeficiency Syndrome (AIDS).
Joel N. Blankson is a professor at the Johns Hopkins School of Medicine in the Department of Medicine, Division of Infectious Diseases. Blankson is an expert on HIV infection, particularly HIV latency and long-term control of HIV infection. He is a lead investigator in studies on these topics and is frequently interviewed in the scientific and popular press. Blankson also practices internal and infectious diseases medicine in Lutherville, Maryland.

DNA dC->dU-editing enzyme APOBEC-3H, also known as Apolipoprotein B mRNA-editing enzyme catalytic polypeptide-like 3H or APOBEC-related protein 10, is a protein that in humans is encoded by the APOBEC3H gene.

The stages of HIV infection are acute infection, latency and AIDS. Acute infection lasts for several weeks and may include symptoms such as fever, swollen lymph nodes, inflammation of the throat, rash, muscle pain, malaise, and mouth and esophageal sores. The latency stage involves few or no symptoms and can last anywhere from two weeks to twenty years or more, depending on the individual. AIDS, the final stage of HIV infection, is defined by low CD4+ T cell counts, various opportunistic infections, cancers and other conditions.
Viral load monitoring for HIV is the regular measurement of the viral load of individual HIV-positive people as part of their personal plan for treatment of HIV/AIDS. A count of the viral load is routine before the start of HIV treatment.

Nonstructural protein 5A (NS5A) inhibitors are direct acting antiviral agents (DAAs) that target viral proteins, and their development was a culmination of increased understanding of the viral life cycle combined with advances in drug discovery technology. However, their mechanism of action is complex and not fully understood. NS5A inhibitors were the focus of much attention when they emerged as a part of the first curative treatment for hepatitis C virus (HCV) infections in 2014. Favorable characteristics have been introduced through varied structural changes, and structural similarities between NS5A inhibitors that are clinically approved are readily apparent. Despite the recent introduction of numerous new antiviral drugs, resistance is still a concern and these inhibitors are therefore always used in combination with other drugs.

Sharon Ruth Lewin, FRACP, FAHMS is the inaugural Director of the Peter Doherty Institute for Infection and Immunity. She is also a Professor of Medicine at The University of Melbourne and a National Health and Medical Research Council (NHMRC) Practitioner Fellow. As an infectious diseases physician and basic scientist, her laboratory focuses on basic, translational and clinical research aimed at finding a cure for HIV and understanding the interaction between HIV and hepatitis B virus. Her laboratory is funded by the NHMRC, the National Institutes of Health, The Wellcome Trust, the American Foundation for AIDS Research and multiple commercial partnerships. She is also the Chief Investigator of a NHMRC Centre of Research Excellence (CRE), The Australian Partnership for Preparedness Research on Infectious Diseases Emergencies (APPRISE) that aims to bring together Australia’s leading experts in clinical, laboratory and public health research to address the key components required for a rapid and effective emergency response to infectious diseases.
Ya-Chi Ho is a Taiwanese infectious disease researcher and Assistant Professor of Assistant Professor of Microbial Pathogenesis and Medicine at Yale University. Her research centers on the interaction between HIV and the host's immune system with the ultimate goal of curing HIV/AIDS.
Francis "Frank" Vincent Chisari is a physician, experimental pathologist, virologist, and immunologist, known for his research on virus-host interactions of hepatitis B and hepatitis C.

Charles Williams Flexner is an American physician, clinical pharmaceutical scientist, academic, author and researcher. He is a Professor of Medicine at the Johns Hopkins University School of Medicine.
References
- ↑ "Vice Chair for Data Integrity and Analytics announced | Medicine Matters". 8 May 2015.
- ↑ ICM affiliated faculty Archived 2012-12-11 at archive.today
- ↑ Stuart Ray's CV, JHU ICM website Archived 2010-06-10 at the Wayback Machine
- ↑ "HIV's Success Might Lie in Its Mutations," United Press International, November 5, 2002.
- ↑ "Sequencing of HIV from India Waves a Red Flag for Vaccine Developers," Gene Therapy Weekly, January 25, 1999.
- ↑ Lole, K. S.; Bollinger, R. C.; Paranjape, R. S.; Gadkari, D.; Kulkarni, S. S.; Novak, N. G.; Ingersoll, R.; Sheppard, H. W.; Ray, S. C. (1999). "Full-length human immunodeficiency virus type 1 genomes from subtype C-infected seroconverters in India, with evidence of intersubtype recombination". Journal of Virology. 73 (1): 152–160. doi:10.1128/JVI.73.1.152-160.1999. PMC 103818 . PMID 9847317.
- ↑ "Small increases or 'blips' in HIV levels do not signal mutations leading to drug-resistant HIV"
- ↑ Kieffer, T.; Finucane, M.; Nettles, R.; Quinn, T.; Broman, K.; Ray, S.; Persaud, D.; Siliciano, R. (2004). "Genotypic analysis of HIV-1 drug resistance at the limit of detection: virus production without evolution in treated adults with undetectable HIV loads". The Journal of Infectious Diseases. 189 (8): 1452–1465. doi: 10.1086/382488 . PMID 15073683.
- ↑ "Rare Case Explains Why Some Infected with HIV Remain Symptom Free without Antiretroviral Drugs" Newswise, August 12, 2008.
- ↑ Bailey, J.; O'Connell, K.; Yang, H.; Han, Y.; Xu, J.; Jilek, B.; Williams, T.; Ray, S.; Siliciano, R.; Blankson, J. N. (2008). "Transmission of human immunodeficiency virus type 1 from a patient who developed AIDS to an elite suppressor". Journal of Virology. 82 (15): 7395–7410. doi:10.1128/JVI.00800-08. PMC 2493308 . PMID 18495769.
- ↑ "Johns Hopkins Team Finds 'Ancestral' Hepatitis-C Virus at Root of Evolution in Acute and Chronic Infections. AScribe, June 9, 2005.
- ↑ Ray, S.; Fanning, L.; Wang, X.; Netski, D.; Kenny-Walsh, E.; Thomas, D. (2005). "Divergent and convergent evolution after a common-source outbreak of hepatitis C virus". The Journal of Experimental Medicine. 201 (11): 1753–1759. doi:10.1084/jem.20050122. PMC 2213258 . PMID 15939791.
- ↑ Dowd, K.; Netski, D.; Wang, X.; Cox, A.; Ray, S. (2009). "Selection pressure from neutralizing antibodies drives sequence evolution during acute infection with hepatitis C virus". Gastroenterology. 136 (7): 2377–2386. doi:10.1053/j.gastro.2009.02.080. PMC 2895772 . PMID 19303013.
- ↑ Wölfl, M.; Rutebemberwa, A.; Mosbruger, T.; Mao, Q.; Li, H. M.; Netski, D.; Ray, S. C.; Pardoll, D.; Sidney, J.; Sette, A.; Allen, T.; Kuntzen, T.; Kavanagh, D. G.; Kuball, J.; Greenberg, P. D.; Cox, A. L. (2008). "Hepatitis C virus immune escape via exploitation of a hole in the T cell repertoire". Journal of Immunology. 181 (9): 6435–6446. doi:10.4049/jimmunol.181.9.6435. PMC 2742502 . PMID 18941234.
- ↑ Rutebemberwa, A.; Ray, S. C.; Astemborski, J.; Levine, J.; Liu, L.; Dowd, K. A.; Clute, S.; Wang, C.; Korman, A.; Sette, A.; Sidney, J.; Pardoll, D. M.; Cox, A. L. (2008). "High-programmed death-1 levels on hepatitis C virus-specific T cells during acute infection are associated with viral persistence and require preservation of cognate antigen during chronic infection". Journal of Immunology. 181 (12): 8215–8225. doi:10.4049/jimmunol.181.12.8215. PMC 2773824 . PMID 19050238.
- ↑ Mao, Q.; Ray, S.; Laeyendecker, O.; Ticehurst, J.; Strathdee, S.; Vlahov, D.; Thomas, D. (2001). "Human immunodeficiency virus seroconversion and evolution of the hepatitis C virus quasispecies". Journal of Virology. 75 (7): 3259–3267. doi:10.1128/JVI.75.7.3259-3267.2001. PMC 114119 . PMID 11238852.
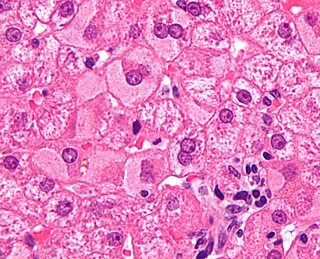
- ↑ Balagopal, A.; Ray, S.; De Oca, R.; Sutcliffe, C.; Vivekanandan, P.; Higgins, Y.; Mehta, S.; Moore, R.; Sulkowski, M.; Thomas, D. L.; Torbenson, M. S. (2009). "Kupffer cells are depleted with HIV immunodeficiency and partially recovered with antiretroviral immune reconstitution". AIDS. 23 (18): 2397–2404. doi:10.1097/QAD.0b013e3283324344. PMC 3092442 . PMID 19773633.
- ↑ Netski, D.; Mao, Q.; Ray, S.; Klein, R. (2008). "Genetic divergence of hepatitis C virus: the role of HIV-related immunosuppression". Journal of Acquired Immune Deficiency Syndromes. 49 (2): 136–141. doi:10.1097/QAI.0b013e3181869a6f. PMC 3071283 . PMID 18769357.
- ↑ Balagopal, A.; Philp, F.; Astemborski, J.; Block, T.; Mehta, A.; Long, R.; Kirk, G.; Mehta, S.; Cox, A.; Thomas, D. L.; Ray, S. C. (2008). "Human immunodeficiency virus-related microbial translocation and progression of hepatitis C". Gastroenterology. 135 (1): 226–233. doi:10.1053/j.gastro.2008.03.022. PMC 2644903 . PMID 18457674.
- ↑ "Hepatitis C: The Insidious Spread Of A Killer Virus" Newsweek, Geoffrey Cowley, April 22, 2002.
- ↑ "The Insidious Spread of a Killer Virus" Newsweek, Anna Kuchment, May 20, 2002.
- ↑ "Johns Hopkins Team Finds 'Ancestral' Hepatitis-C Virus At The Root Of Evolution In Infections" ScienceDaily, June 10, 2005.
- ↑ Stuart Ray's profile at the American Society for Clinical Investigation