Related Research Articles
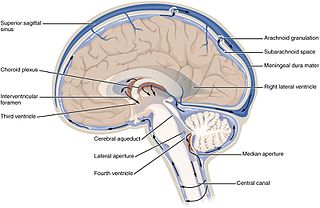
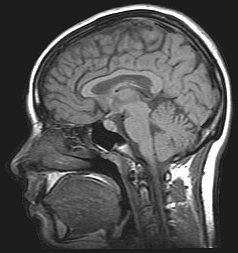
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found in the brain and spinal cord. It is produced by specialised ependymal cells in the choroid plexuses of the ventricles of the brain, and absorbed in the arachnoid granulations. There is about 125 mL of CSF at any one time, and about 500 mL is generated every day. CSF acts as a cushion or buffer, providing basic mechanical and immunological protection to the brain inside the skull. CSF also serves a vital function in the cerebral autoregulation of cerebral blood flow.
Idiopathic intracranial hypertension (IIH), previously known as pseudotumor cerebri and benign intracranial hypertension, is a condition characterized by increased intracranial pressure without a detectable cause. The main symptoms are headache, vision problems, ringing in the ears with the heartbeat, and shoulder pain. Complications may include vision loss.

The cauda equina is a bundle of spinal nerves and spinal nerve rootlets, consisting of the second through fifth lumbar nerve pairs, the first through fifth sacral nerve pairs, and the coccygeal nerve, all of which arise from the lumbar enlargement and the conus medullaris of the spinal cord. The cauda equina occupies the lumbar cistern, a subarachnoid space inferior to the conus medullaris. The nerves that compose the cauda equina innervate the pelvic organs and lower limbs to include motor innervation of the hips, knees, ankles, feet, internal anal sphincter and external anal sphincter. In addition, the cauda equina extends to sensory innervation of the perineum and, partially, parasympathetic innervation of the bladder.

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia performed by anesthesiologists and nurse anesthetists which can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic or opioid injected into the cerebrospinal fluid provides anesthesia, analgesia, and motor and sensory blockade. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

Epidural administration is a method of administration in which a drug is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration is often accomplished through use of a catheter placed into the epidural space. The technique of epidural administration was first described in 1921 by Spanish military surgeon Fidel Pagés.

Aseptic meningitis is the inflammation of the meninges, a membrane covering the brain and spinal cord, in patients whose cerebral spinal fluid test result is negative with routine bacterial cultures. Aseptic meningitis is caused by viruses, mycobacteria, spirochetes, fungi, medications, and cancer malignancies. The testing for both meningitis and aseptic meningitis is mostly the same. A cerebrospinal fluid sample is taken by lumbar puncture and is tested for leukocyte levels to determine if there is an infection and goes on to further testing to see what the actual cause is. The symptoms are the same for both meningitis and aseptic meningitis but the severity of the symptoms and the treatment can depend on the certain cause.
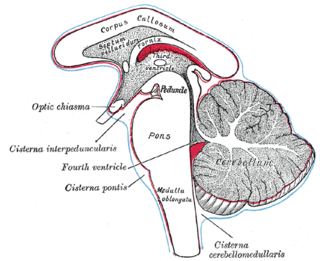
The subarachnoid cisterns are spaces formed by openings in the subarachnoid space, an anatomic space in the meninges of the brain. The space separates two of the meninges, the arachnoid mater and the pia mater. These cisterns are filled with cerebrospinal fluid.

Dandy–Walker malformation (DWM), also known as Dandy–Walker syndrome (DWS), is a rare congenital brain malformation in which the part joining the two hemispheres of the cerebellum does not fully form, and the fourth ventricle and space behind the cerebellum are enlarged with cerebrospinal fluid. Most of those affected develop hydrocephalus within the first year of life, which can present as increasing head size, vomiting, excessive sleepiness, irritability, downward deviation of the eyes and seizures. Other, less common symptoms are generally associated with comorbid genetic conditions and can include congenital heart defects, eye abnormalities, intellectual disability, congenital tumours, other brain defects such as agenesis of the corpus callosum, skeletal abnormalities, an occipital encephalocele or underdeveloped genitalia or kidneys. It is sometimes discovered in adolescents or adults due to mental health problems.
Myelography is a type of radiographic examination that uses a contrast medium to detect pathology of the spinal cord, including the location of a spinal cord injury, cysts, and tumors. Historically the procedure involved the injection of a radiocontrast agent into the cervical or lumbar spine, followed by several X-ray projections. Today, myelography has largely been replaced by the use of MRI scans, although the technique is still sometimes used under certain circumstances – though now usually in conjunction with CT rather than X-ray projections.
A radionuclide cisternogram is a medical imaging study which involves injecting a radionuclide by lumbar puncture into a patient's cerebral spinal fluid (CSF) to determine if there is abnormal CSF flow within the brain and spinal canal which can be altered by hydrocephalus, Arnold–Chiari malformation, syringomyelia, or an arachnoid cyst. It may also evaluate a suspected leak from the CSF cavity into the nasal cavity. A leak can also be confirmed by the presence of beta-2 transferrin in fluid collected from the nose before this more invasive procedure is performed.

A laminotomy is an orthopaedic neurosurgical procedure that removes part of the lamina of a vertebral arch in order to relieve pressure in the vertebral canal. A laminotomy is less invasive than conventional vertebral column surgery techniques, such as laminectomy because it leaves more ligaments and muscles attached to the vertebral column intact and it requires removing less bone from the vertebra. As a result, laminotomies typically have a faster recovery time and result in fewer postoperative complications. Nevertheless, possible risks can occur during or after the procedure like infection, hematomas, and dural tears. Laminotomies are commonly performed as treatment for lumbar spinal stenosis and herniated disks. MRI and CT scans are often used pre- and post surgery to determine if the procedure was successful.

Leptomeningeal cancer is a rare complication of cancer in which the disease spreads from the original tumor site to the meninges surrounding the brain and spinal cord. This leads to an inflammatory response, hence the alternative names neoplastic meningitis (NM), malignant meningitis, or carcinomatous meningitis. The term leptomeningeal describes the thin meninges, the arachnoid and the pia mater, between which the cerebrospinal fluid is located. The disorder was originally reported by Eberth in 1870.
Post-dural-puncture headache (PDPH) is a complication of puncture of the dura mater. The headache is severe and described as "searing and spreading like hot metal", involving the back and front of the head and spreading to the neck and shoulders, sometimes involving neck stiffness. It is exacerbated by movement and sitting or standing and is relieved to some degree by lying down. Nausea, vomiting, pain in arms and legs, hearing loss, tinnitus, vertigo, dizziness and paraesthesia of the scalp are also common.

An epidural blood patch is a surgical procedure that uses autologous blood in order to close one or many holes in the dura mater of the spinal cord, usually as a result of a previous lumbar puncture. The procedure can be used to relieve post dural puncture headaches caused by lumbar puncture. A small amount of the patient's blood is injected into the epidural space near the site of the original puncture; the resulting blood clot then "patches" the meningeal leak. The procedure carries the typical risks of any epidural puncture. However, even though it is often effective, further intervention is sometimes necessary.

A spontaneous cerebrospinal fluid leak is a cerebrospinal fluid leak – a leak of cerebrospinal fluid that surrounds the brain and spinal cord from the protective dural sac for no apparent reason. The dura mater is the tough, outermost of layer of the meninges, the membranes surrounding the brain and spinal cord.

Metrizamide is a non-ionic iodine-based radiocontrast agent. A density gradient medium for the centrifugation of biological particles.

The spinal cord is a long, thin, tubular structure made up of nervous tissue, which extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column. It encloses the central canal of the spinal cord, which contains cerebrospinal fluid. The brain and spinal cord together make up the central nervous system (CNS). In humans, the spinal cord begins at the occipital bone, passing through the foramen magnum and entering the spinal canal at the beginning of the cervical vertebrae. The spinal cord extends down to between the first and second lumbar vertebrae, where it ends. The enclosing bony vertebral column protects the relatively shorter spinal cord. It is around 45 cm (18 in) in men and around 43 cm (17 in) long in women. The diameter of the spinal cord ranges from 13 mm in the cervical and lumbar regions to 6.4 mm in the thoracic area.
A lumbar–peritoneal shunt is a technique to channelise the cerebrospinal fluid (CSF) from the lumbar thecal sac into the peritoneal cavity.

The thecal sac or dural sac is the membranous sheath (theca) or tube of dura mater that surrounds the spinal cord and the cauda equina. The thecal sac contains the cerebrospinal fluid which provides nutrients and buoyancy to the spinal cord. From the skull the tube adheres to bone at the foramen magnum and extends down to the second sacral vertebra where it tapers to cover over the filum terminale. Along most of the spinal canal it is separated from the inner surface by the epidural space. The sac has projections that follow the spinal nerves along their paths out of the vertebral canal which become the dural root sheaths.
References
- Marco Mumenthaler; Heinrich Mattle (1 January 2011). Neurology. Thieme. pp. 79–80. ISBN 978-1-60406-135-2.