Related Research Articles

Henry Gustav Molaison, known widely as H.M., was an American who had a bilateral medial temporal lobectomy to surgically resect the anterior two thirds of his hippocampi, parahippocampal cortices, entorhinal cortices, piriform cortices, and amygdalae in an attempt to cure his epilepsy. Although the surgery was partially successful in controlling his epilepsy, a severe side effect was that he became unable to form new memories.

The temporal lobe is one of the four major lobes of the cerebral cortex in the brain of mammals. The temporal lobe is located beneath the lateral fissure on both cerebral hemispheres of the mammalian brain.
The Wada test, also known as the intracarotid sodium amobarbital procedure (ISAP), establishes cerebral language and memory representation of each hemisphere.
Corpus callosotomy is a palliative surgical procedure for the treatment of medically refractory epilepsy. In this procedure the corpus callosum is cut through in an effort to limit the spread of epileptic activity between the two halves of the brain.

Hippocampal sclerosis (HS) or mesial temporal sclerosis (MTS) is a neuropathological condition with severe neuronal cell loss and gliosis in the hippocampus. Neuroimaging tests such as magnetic resonance imaging (MRI) and positron emission tomography (PET) may identify individuals with hippocampal sclerosis. Hippocampal sclerosis occurs in 3 distinct settings: mesial temporal lobe epilepsy, adult neurodegenerative disease and acute brain injury.

In the field of neurology, temporal lobe epilepsy is an enduring brain disorder that causes unprovoked seizures from the temporal lobe. Temporal lobe epilepsy is the most common type of focal onset epilepsy among adults. Seizure symptoms and behavior distinguish seizures arising from the medial temporal lobe from seizures arising from the lateral (neocortical) temporal lobe. Memory and psychiatric comorbidities may occur. Diagnosis relies on electroencephalographic (EEG) and neuroimaging studies. Anticonvulsant medications, epilepsy surgery and dietary treatments may improve seizure control.
Frontal lobe epilepsy (FLE) is a neurological disorder that is characterized by brief, recurring seizures arising in the frontal lobes of the brain, that often occur during sleep. It is the second most common type of epilepsy after temporal lobe epilepsy (TLE), and is related to the temporal form in that both forms are characterized by partial (focal) seizures.
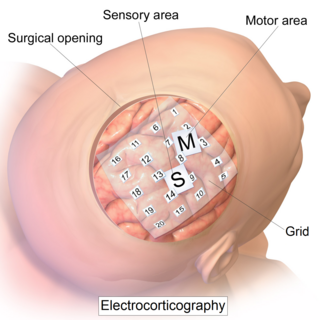
Electrocorticography (ECoG), a type of intracranial electroencephalography (iEEG), is a type of electrophysiological monitoring that uses electrodes placed directly on the exposed surface of the brain to record electrical activity from the cerebral cortex. In contrast, conventional electroencephalography (EEG) electrodes monitor this activity from outside the skull. ECoG may be performed either in the operating room during surgery or outside of surgery. Because a craniotomy is required to implant the electrode grid, ECoG is an invasive procedure.

Foix–Chavany–Marie Syndrome (FCMS), also known as bilateral opercular syndrome, is a neuropathological disorder characterized by paralysis of the facial, tongue, pharynx, and masticatory muscles of the mouth that aid in chewing. The disorder is primarily caused by thrombotic and embolic strokes, which cause a deficiency of oxygen in the brain. As a result, bilateral lesions may form in the junctions between the frontal lobe and temporal lobe, the parietal lobe and cortical lobe, or the subcortical region of the brain. FCMS may also arise from defects existing at birth that may be inherited or nonhereditary. Symptoms of FCMS can be present in a person of any age and it is diagnosed using automatic-voluntary dissociation assessment, psycholinguistic testing, neuropsychological testing, and brain scanning. Treatment for FCMS depends on the onset, as well as on the severity of symptoms, and it involves a multidisciplinary approach.
Epilepsy surgery involves a neurosurgical procedure where an area of the brain involved in seizures is either resected, ablated, disconnected or stimulated. The goal is to eliminate seizures or significantly reduce seizure burden. Approximately 60% of all people with epilepsy have focal epilepsy syndromes. In 15% to 20% of these patients, the condition is not adequately controlled with anticonvulsive drugs. Such patients are potential candidates for surgical epilepsy treatment.

Dysembryoplastic neuroepithelial tumour is a type of brain tumor. Most commonly found in the temporal lobe, DNTs have been classified as benign tumours. These are glioneuronal tumours comprising both glial and neuron cells and often have ties to focal cortical dysplasia.
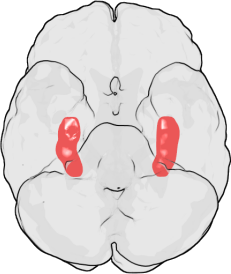
Amygdalohippocampectomy is a surgical procedure for the treatment of epilepsy. It consists of the removal of the hippocampus, which has a role in memory, spatial awareness, and navigation, and the amygdalae, which have a role in the processing and memory of emotional reactions, both structures forming part of the limbic system of the brain.
Transient epileptic amnesia (TEA) is a rare but probably underdiagnosed neurological condition which manifests as relatively brief and generally recurring episodes of amnesia caused by underlying temporal lobe epilepsy. Though descriptions of the condition are based on fewer than 100 cases published in the medical literature, and the largest single study to date included 50 people with TEA, TEA offers considerable theoretical significance as competing theories of human memory attempt to reconcile its implications.
Amnesia is a deficit in memory caused by brain damage or brain diseases, but it can also be temporarily caused by the use of various sedatives and hypnotic drugs. The memory can be either wholly or partially lost due to the extent of damage that was caused.

Epilepsy is a neurological condition of recurrent episodes of unprovoked epileptic seizures. A seizure is an abnormal neuronal brain activity that can cause intellectual, emotional, and social consequences. Epilepsy affects children and adults of all ages and races, it is one of the most common neurological disorders of the nervous system. As well as, this condition is more common among children than adults affecting about 6 out of 1000 US children that are between the age of 0 to 5 years old. The epileptic seizures can be of different types depending on the part of the brain that was affected, seizures are classified in 2 main types partial seizure or genralized seizure.
Drug-resistant epilepsy (DRE), also known as refractory epilepsy, intractable epilepsy, or pharmacoresistant epilepsy, is diagnosed following a failure of adequate trials of two tolerated and appropriately chosen and used antiepileptic drugs (AEDs) to achieve sustained seizure freedom. The probability that the next medication will achieve seizure freedom drops with every failed AED. For example, after two failed AEDs, the probability that the third will achieve seizure freedom is around 4%. Drug-resistant epilepsy is commonly diagnosed after several years of uncontrolled seizures, however, in most cases, it is evident much earlier. Approximately 30% of people with epilepsy have a drug-resistant form.
Musicogenic seizure, also known as music-induced seizure, is a rare type of seizure, with an estimated prevalence of 1 in 10,000,000 individuals, that arises from disorganized or abnormal brain electrical activity when a person hears or is exposed to a specific type of sound or musical stimuli. There are challenges when diagnosing a music-induced seizure due to the broad scope of triggers, and time delay between a stimulus and seizure. In addition, the causes of musicogenic seizures are not well-established as solely limited cases and research have been discovered and conducted respectively. Nevertheless, the current understanding of the mechanism behind musicogenic seizure is that music triggers the part of the brain that is responsible for evoking an emotion associated with that music. Dysfunction in this system leads to an abnormal release of dopamine, eventually inducing seizure.
Amygdalotomy is a form of psychosurgery which involves the surgical removal or destruction of the amygdala, or parts of the amygdala. It is usually a last-resort treatment for severe aggressive behavioral disorders and similar behaviors including hyperexcitability, violent outbursts, and self-mutilation. The practice of medical amygdalotomy typically involves the administration of general anesthesia and is achieved through the application of cranial stereotactic surgery to target regions of the amygdala for surgical destruction. While some studies have found stereotactic amygdalotomy in humans to be an effective treatment for severe cases of intractable aggressive behavior that has not responded to standard treatment methods, other studies remain inconclusive. In most cases of amygdalotomy in humans, there is no substantial evidence of impairment in overall cognitive function, including intelligence and working memory, however, deficits in specific areas of memory have been noted pertaining to the recognition and emotional interpretation of facial stimuli. This is because there are specialized cells in the amygdala which attend to facial stimuli.
Christine Kilpatrick is an Australian neurologist and the chief executive of Royal Melbourne Health. She has held this position since 2017. Previously, she was the chief executive of the Royal Children's Hospital from 2008 to 2017 and the executive director of Medical Services, Melbourne Health and executive director of the Royal Melbourne Hospital from 2004 to 2008. Before she held these positions, she worked as a neurologist at Royal Melbourne Health and engaged in extensive neurological research, especially epilepsy.

Elaine Wyllie is a professor of neurology at the Cleveland Clinic Lerner College of Medicine and staff physician in Cleveland Clinic's Epilepsy Center. Her research focuses on the role of epilepsy surgery in children with drug-resistant seizures.
References
- ↑ "Epilepsy surgery, Temporal lobectomy, Vagus Nerve Stimulation". Cincinnati Ohio Mayfield Brain & Spine. Retrieved 20 January 2022.
- ↑ "Wada Test". Epilepsy Foundation. Retrieved 20 January 2022.
- ↑ Bonilha, Leonardo; Yasuda, Clarissa Lin; Rorden, Chris; Li, Li M.; Tedeschi, Helder; de Oliveira, Evandro; Cendes, Fernando (March 2007). "Does resection of the medial temporal lobe improve the outcome of temporal lobe epilepsy surgery?". Epilepsia. 48 (3): 571–578. doi: 10.1111/j.1528-1167.2006.00958.x . ISSN 0013-9580. PMID 17326795. S2CID 25692616.
- ↑ "Anteromedial Temporal Lobectomy". Neurosurgical Atlas. Retrieved 20 January 2022.
- ↑ Engel J (March 1996). "Surgery for seizures". The New England Journal of Medicine. 334 (10): 647–652. doi:10.1056/nejm199603073341008. PMID 8592530.
- ↑ Spencer SS, Berg AT, Vickrey BG, Sperling MR, Bazil CW, Shinnar S, Langfitt JT, Walczak TS, Pacia SV (September 2005). "Predicting long-term seizure outcome after resective epilepsy surgery: the multicenter study". Neurology. 65 (6): 912–918. doi:10.1212/01.wnl.0000176055.45774.71. PMID 16186534. S2CID 24280239.
- ↑ "anterior_temporal_lobectomy". Operative Neurosurgery. Retrieved 7 January 2022.
- ↑ Wiebe S, Blume WT, Girvin JP, Eliasziw M (August 2001). "A randomized, controlled trial of surgery for temporal-lobe epilepsy". The New England Journal of Medicine. 345 (5): 311–318. doi: 10.1056/NEJM200108023450501 . PMID 11484687. S2CID 31539171.
- ↑ Muzumdar, Dattatraya; Patil, Manoj; Goel, Atul; Ravat, Sangeeta; Sawant, Nina; Shah, Urvashi (1 December 2016). "Mesial temporal lobe epilepsy – An overview of surgical techniques". International Journal of Surgery. Epilepsy surgery for pharmacoresistant epilepsy. 36 (Pt B): 411–419. doi: 10.1016/j.ijsu.2016.10.027 . ISSN 1743-9191. PMID 27773861.
- ↑ "Recovery and Life After Surgery". Epilepsy Foundation. Retrieved 7 January 2022.
- ↑ Vermathen, P.; Ende, G.; Laxer, K. D.; Walker, J. A.; Knowlton, R. C.; Barbaro, N. M.; Matson, G. B.; Weiner, M. W. (27 August 2002). "Temporal lobectomy for epilepsy: Recovery of the contralateral hippocampus measured by 1H MRS". Neurology. 59 (4): 633–636. doi:10.1212/wnl.59.4.633. ISSN 0028-3878. PMC 2753242 . PMID 12196667.
- ↑ Van Gompel, Jamie J.; Ottman, Ruth; Worrell, Gregory A.; Marsh, W. Richard; Wetjen, Nicholas M.; Cascino, Gregory D.; Meyer, Fredric B. (November 2012). "Use of Anterior Temporal Lobectomy for Epilepsy in a Community-Based Population". Archives of Neurology. 69 (11): 1476–1481. doi:10.1001/archneurol.2012.1200. ISSN 0003-9942. PMC 3526693 . PMID 22911042.