Neurosurgery or neurological surgery, known in common parlance as brain surgery, is the medical specialty concerned with the surgical treatment of disorders which affect any portion of the nervous system including the brain, spinal cord and peripheral nervous system.

The corpus callosum, also callosal commissure, is a wide, thick nerve tract, consisting of a flat bundle of commissural fibers, beneath the cerebral cortex in the brain. The corpus callosum is only found in placental mammals. It spans part of the longitudinal fissure, connecting the left and right cerebral hemispheres, enabling communication between them. It is the largest white matter structure in the human brain, about 10 in (250 mm) in length and consisting of 200–300 million axonal projections.

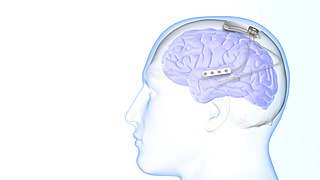
Deep brain stimulation (DBS) is a surgical procedure that implants a neurostimulator and electrodes which sends electrical impulses to specified targets in the brain responsible for movement control. The treatment is designed for a range of movement disorders such as Parkinson's disease, essential tremor, and dystonia, as well as for certain neuropsychiatric conditions like obsessive-compulsive disorder (OCD) and epilepsy. The exact mechanisms of DBS are complex and not entirely clear, but it is known to modify brain activity in a structured way.

Split-brain or callosal syndrome is a type of disconnection syndrome when the corpus callosum connecting the two hemispheres of the brain is severed to some degree. It is an association of symptoms produced by disruption of, or interference with, the connection between the hemispheres of the brain. The surgical operation to produce this condition involves transection of the corpus callosum, and is usually a last resort to treat refractory epilepsy. Initially, partial callosotomies are performed; if this operation does not succeed, a complete callosotomy is performed to mitigate the risk of accidental physical injury by reducing the severity and violence of epileptic seizures. Before using callosotomies, epilepsy is instead treated through pharmaceutical means. After surgery, neuropsychological assessments are often performed.

The longitudinal fissure is the deep groove that separates the two cerebral hemispheres of the vertebrate brain. Lying within it is a continuation of the dura mater called the falx cerebri. The inner surfaces of the two hemispheres are convoluted by gyri and sulci just as is the outer surface of the brain.

Lennox–Gastaut syndrome (LGS) is a complex, rare, and severe childhood-onset epilepsy syndrome. It is characterized by multiple and concurrent seizure types including tonic seizure, cognitive dysfunction, and slow spike waves on electroencephalogram (EEG), which are very abnormal. Typically, it presents in children aged 3–5 years and most of the time persists into adulthood with slight changes in the electroclinical phenotype. It has been associated with perinatal injuries, congenital infections, brain malformations, brain tumors, genetic disorders such as tuberous sclerosis and numerous gene mutations. Sometimes LGS is observed after infantile epileptic spasm syndrome. The prognosis for LGS is marked by a 5% mortality in childhood and persistent seizures into adulthood.

Vagus nerve stimulation (VNS) is a medical treatment that involves delivering electrical impulses to the vagus nerve. It is used as an add-on treatment for certain types of intractable epilepsy, cluster headaches, treatment-resistant depression and stroke rehabilitation.

In the field of neurology, temporal lobe epilepsy is an enduring brain disorder that causes unprovoked seizures from the temporal lobe. Temporal lobe epilepsy is the most common type of focal onset epilepsy among adults. Seizure symptoms and behavior distinguish seizures arising from the medial temporal lobe from seizures arising from the lateral (neocortical) temporal lobe. Memory and psychiatric comorbidities may occur. Diagnosis relies on electroencephalographic (EEG) and neuroimaging studies. Anticonvulsant medications, epilepsy surgery and dietary treatments may improve seizure control.
Frontal lobe epilepsy (FLE) is a neurological disorder that is characterized by brief, recurring seizures arising in the frontal lobes of the brain, that often occur during sleep. It is the second most common type of epilepsy after temporal lobe epilepsy (TLE), and is related to the temporal form in that both forms are characterized by partial (focal) seizures.
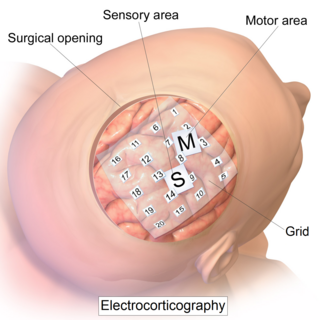
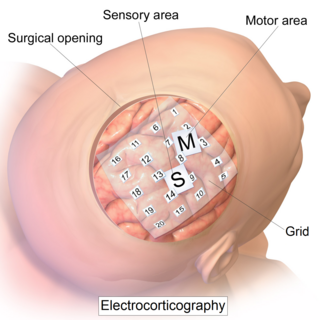
Electrocorticography (ECoG), a type of intracranial electroencephalography (iEEG), is a type of electrophysiological monitoring that uses electrodes placed directly on the exposed surface of the brain to record electrical activity from the cerebral cortex. In contrast, conventional electroencephalography (EEG) electrodes monitor this activity from outside the skull. ECoG may be performed either in the operating room during surgery or outside of surgery. Because a craniotomy is required to implant the electrode grid, ECoG is an invasive procedure.
Anterior temporal lobectomy is the complete or partial removal of the anterior portion of the temporal lobe of the brain. The exact boundaries for removal can vary slightly in practice and between neurosurgeons. It is a treatment option for temporal lobe epilepsy for those in whom anticonvulsant medications do not control epileptic seizures, and who have frequent seizures, and who additionally qualify based on a WADA test to localize the dominant hemisphere for language module.
Juvenile myoclonic epilepsy (JME), also known as Janz syndrome or impulsive petit mal, is a form of hereditary, idiopathic generalized epilepsy, representing 5–10% of all epilepsy cases. Typically it first presents between the ages of 12 and 18 with myoclonic seizures. These events typically occur after awakening from sleep, during the evening or when sleep-deprived. JME is also characterized by generalized tonic–clonic seizures, and a minority of patients have absence seizures. It was first described by Théodore Herpin in 1857. Understanding of the genetics of JME has been rapidly evolving since the 1990s, and over 20 chromosomal loci and multiple genes have been identified. Given the genetic and clinical heterogeneity of JME some authors have suggested that it should be thought of as a spectrum disorder.
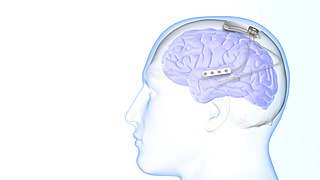
Responsive neurostimulation device is a medical device that senses changes in a person's body and uses neurostimulation to respond in the treatment of disease. The FDA has approved devices for use in the United States in the treatment of epileptic seizures and chronic pain conditions. Devices are being studied for use in the treatment of essential tremor, Parkinson's disease, Tourette's syndrome, depression, obesity, and post-traumatic stress disorder.

Epilepsy is a neurological condition of recurrent episodes of unprovoked epileptic seizures. A seizure is an abnormal neuronal brain activity that can cause intellectual, emotional, and social consequences. Epilepsy affects children and adults of all ages and races, it is one of the most common neurological disorders of the nervous system. As well as, this condition is more common among children than adults affecting about 6 out of 1000 US children that are between the age of 0 to 5 years old. The epileptic seizures can be of different types depending on the part of the brain that was affected, seizures are classified in 2 main types partial seizure or genralized seizure.
Cortical stimulation mapping (CSM) is a type of electrocorticography that involves a physically invasive procedure and aims to localize the function of specific brain regions through direct electrical stimulation of the cerebral cortex. It remains one of the earliest methods of analyzing the brain and has allowed researchers to study the relationship between cortical structure and systemic function. Cortical stimulation mapping is used for a number of clinical and therapeutic applications, and remains the preferred method for the pre-surgical mapping of the motor cortex and language areas to prevent unnecessary functional damage. There are also some clinical applications for cortical stimulation mapping, such as the treatment of epilepsy.
Neuromodulation is "the alteration of nerve activity through targeted delivery of a stimulus, such as electrical stimulation or chemical agents, to specific neurological sites in the body". It is carried out to normalize – or modulate – nervous tissue function. Neuromodulation is an evolving therapy that can involve a range of electromagnetic stimuli such as a magnetic field (rTMS), an electric current, or a drug instilled directly in the subdural space. Emerging applications involve targeted introduction of genes or gene regulators and light (optogenetics), and by 2014, these had been at minimum demonstrated in mammalian models, or first-in-human data had been acquired. The most clinical experience has been with electrical stimulation.
Dual consciousness is a theoretical concept in neuroscience. It is proposed that it is possible that a person may develop two separate conscious entities within their one brain after undergoing a corpus callosotomy. The idea first began circulating in the neuroscience community after some split-brain patients exhibited the alien hand syndrome, which led some scientists to believe that there must be two separate consciousnesses within the brain's left and right hemispheres in competition with one another once the corpus callosum is severed.
Drug-resistant epilepsy (DRE), also known as refractory epilepsy, intractable epilepsy, or pharmacoresistant epilepsy, is diagnosed following a failure of adequate trials of two tolerated and appropriately chosen and used antiepileptic drugs (AEDs) to achieve sustained seizure freedom. The probability that the next medication will achieve seizure freedom drops with every failed AED. For example, after two failed AEDs, the probability that the third will achieve seizure freedom is around 4%. Drug-resistant epilepsy is commonly diagnosed after several years of uncontrolled seizures, however, in most cases, it is evident much earlier. Approximately 30% of people with epilepsy have a drug-resistant form.
Musicogenic seizure, also known as music-induced seizure, is a rare type of seizure, with an estimated prevalence of 1 in 10,000,000 individuals, that arises from disorganized or abnormal brain electrical activity when a person hears or is exposed to a specific type of sound or musical stimuli. There are challenges when diagnosing a music-induced seizure due to the broad scope of triggers, and time delay between a stimulus and seizure. In addition, the causes of musicogenic seizures are not well-established as solely limited cases and research have been discovered and conducted respectively. Nevertheless, the current understanding of the mechanism behind musicogenic seizure is that music triggers the part of the brain that is responsible for evoking an emotion associated with that music. Dysfunction in this system leads to an abnormal release of dopamine, eventually inducing seizure.

Sandi Lam is a Canadian pediatric neurosurgeon and is known for her research in minimally invasive endoscopic hemispherectomy for patients with epilepsy. Lam is the Vice Chair for Pediatric Neurological Surgery at Northwestern University and the Division Chief of Pediatric Neurosurgery at Lurie Children's Hospital. She has spent her career advancing pediatric brain surgery capabilities globally through her work in Kenya performing surgeries as well as training and mentoring local residents and fellows.