A bunion, also known as hallux valgus, is a deformity of the MTP joint connecting the big toe to the foot. The big toe often bends towards the other toes and the joint becomes red and painful. The onset of bunions is typically gradual. Complications may include bursitis or arthritis.

The navicular bone is a small bone found in the feet of most mammals.

Diseases of the foot generally are not limited, that is they are related to or manifest elsewhere in the body. However, the foot is often the first place some of these diseases or a sign or symptom of others appear. This is because of the foot's distance from the central circulation, the heart and its constant exposure to pressures from the ground and the weight of the body.

Flat feet, also called pes planus or fallen arches, is a postural deformity in which the arches of the foot collapse, with the entire sole of the foot coming into complete or near-complete contact with the ground. Sometimes children are born with flat feet (congenital). There is a functional relationship between the structure of the arch of the foot and the biomechanics of the lower leg. The arch provides an elastic, springy connection between the forefoot and the hind foot so that a majority of the forces incurred during weight bearing on the foot can be dissipated before the force reaches the long bones of the leg and thigh.

The tibialis posterior muscle is the most central of all the leg muscles, and is located in the deep posterior compartment of the leg. It is the key stabilizing muscle of the lower leg.

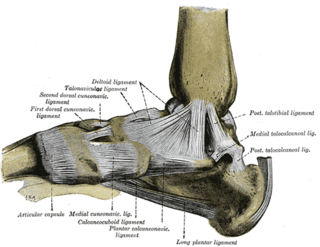
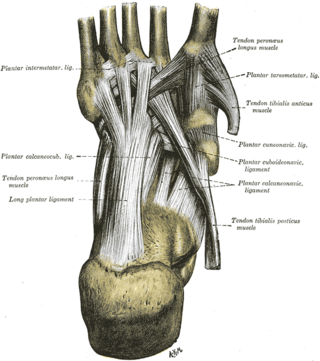
Tarsal tunnel syndrome (TTS) is a nerve compression syndrome or nerve entrapment syndrome causing a painful foot condition in which the tibial nerve is entrapped as it travels through the tarsal tunnel. The tarsal tunnel is found along the inner leg behind the medial malleolus. The posterior tibial artery, tibial nerve, and tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles travel in a bundle through the tarsal tunnel. Inside the tunnel, the nerve splits into three segments. One nerve (calcaneal) continues to the heel, the other two continue on to the bottom of the foot. The tarsal tunnel is delineated by bone on the inside and the flexor retinaculum on the outside.

Köhler disease is a rare bone disorder of the foot found in children between six and nine years of age. The disease typically affects boys, but it can also affect girls. It was first described in 1908 by Alban Köhler (1874–1947), a German radiologist. Dr. A. Köhler noted that children with foot pain displayed characteristics, within their x-rays, of irregularity in growth and development of the tarsal navicular bone in the foot. Furthermore, Köhler disease is known to affect five times more boys than girls and typically, only one foot is affected. The disease was then found to belong to a group of conditions called osteochondroses, which disturb bone growth at ossification centres which occurs during bone development.

Morton's neuroma is a benign neuroma of an intermetatarsal plantar nerve, most commonly of the second and third intermetatarsal spaces, which results in the entrapment of the affected nerve. The main symptoms are pain and/or numbness, sometimes relieved by ceasing to wear footwear with tight toe boxes and high heels. The condition is named after Thomas George Morton, though it was first correctly described by a chiropodist named Durlacher.
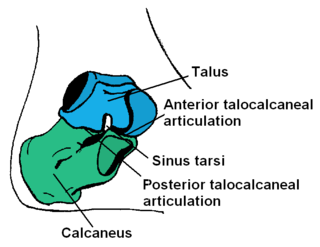
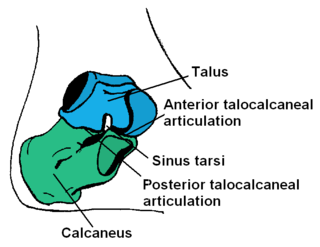
In human anatomy, the subtalar joint, also known as the talocalcaneal joint, is a joint of the foot. It occurs at the meeting point of the talus and the calcaneus.
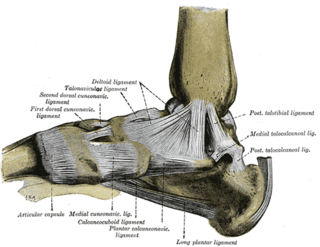
The cuneonavicular joint is a joint (articulation) in the human foot. It is formed between the navicular bone and the three cuneiform bones. The navicular and cuneiform bones are connected by dorsal and plantar ligaments.
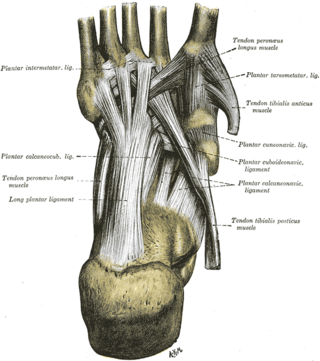
The cuboideonavicular joint is a joint (articulation) in the foot formed between the navicular bone and cuboid bone. The navicular bone is connected with the cuboid bone by the dorsal, plantar, and interosseous cuboideonavicular ligaments. It is a syndesmosis type fibrous joint.

Synostosis is fusion of two or more bones. It can be normal in puberty, or abnormal. When synostosis is abnormal it is a type of dysostosis. Examples of synostoses include:

An accessory navicular bone is an accessory bone of the foot that occasionally develops abnormally in front of the ankle towards the inside of the foot. This bone may be present in approximately 2-21% of the general population and is usually asymptomatic. When it is symptomatic, surgery may be necessary.
Foot and ankle surgery is a sub-specialty of orthopedics and podiatry that deals with the treatment, diagnosis and prevention of disorders of the foot and ankle. Orthopaedic surgeons are medically qualified, having been through four years of college, followed by 4 years of medical school or osteopathic medical school to obtain an M.D. or D.O. followed by specialist training as a resident in orthopaedics, and only then do they sub-specialise in foot and ankle surgery. Training for a podiatric foot and ankle surgeon consists of four years of college, four years of podiatric medical school (D.P.M.), 3–4 years of a surgical residency and an optional 1 year fellowship.

Pigeon toe, also known as in-toeing, is a condition which causes the toes to point inward when walking. It is most common in infants and children under two years of age and, when not the result of simple muscle weakness, normally arises from underlying conditions, such as a twisted shin bone or an excessive anteversion resulting in the twisting of the thigh bone when the front part of a person's foot is turned in.
Unlike the flexible flat foot that is commonly encountered in young children, congenital vertical talus is characterized by presence of a very rigid foot deformity. The foot deformity in congenital vertical talus consists of various components, namely a prominent calcaneus caused by the ankle equines or plantar flexion, a convex and rounded sole of the foot caused by prominence of the head of the talus, and a dorsiflexion and abduction of the forefoot and midfoot on the hindfoot. It gets its name from the foot's resemblance to the bottom of a rocking chair. There are two subcategories of congenital vertical talus; namely idiopathic or isolated type, and non-idiopathic type, which may be seen in association with arthrogryposis multiplex congenital, genetic syndromes and other neuromuscular disorders.

Mueller–Weiss syndrome, also known as Mueller–Weiss disease, is a rare idiopathic degenerative disease of the adult navicular bone characterized by progressive collapse and fragmentation, leading to mid- and hindfoot pain and deformity. It is most commonly seen in females, ages 40–60. Characteristic imaging shows lateral navicular collapse. This disease had been historically considered to be a form of adult onset osteonecrosis, with blood flow cutoff to the navicular.

Sinus tarsi syndrome is the clinical disorder of pain and tenderness in the sinus tarsi, which is a lateral tunnel in the foot at the junction of the hindfoot and the midfoot, between the ankle and the heel. Most of the time, sinus tarsi syndrome onsets after ankle sprains, however there can be other causes. There are a variety of treatments, divided into conservative treatments such as physical and orthotic therapy, and more invasive ones such as cortisone injections. The condition is somewhat poorly understood and is subject to heavy debate in the medical community.
Posterior tibial tendon dysfunction is the dysfunction of the posterior tibial tendon. It is a progressive disease that has four stages and is the most common cause of adult flatfoot.
Subtalar arthroereisis is a common treatment for symptomatic pes planus, also known as flatfoot. There are two forms of pes planus: rigid flatfoot (RFF) and flexible flatfoot (FFF). The symptoms of the former typically necessitate surgical intervention. The latter may manifest fatigue or pain, but is typically asymptomatic.