A central venous catheter (CVC), also known as a central line (c-line), central venous line, or central venous access catheter, is a catheter placed into a large vein. It is a form of venous access. Placement of larger catheters in more centrally located veins is often needed in critically ill patients, or in those requiring prolonged intravenous therapies, for more reliable vascular access. These catheters are commonly placed in veins in the neck, chest, groin, or through veins in the arms.
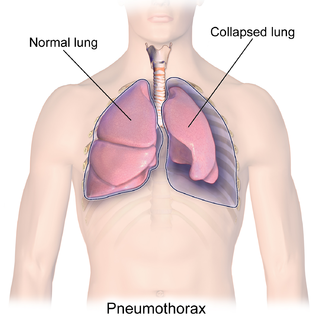
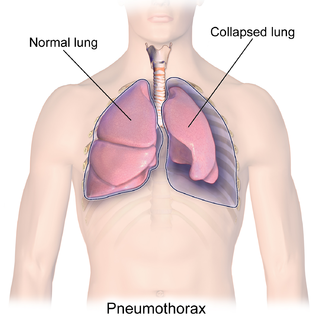
A pneumothorax is an abnormal collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and shortness of breath. In a minority of cases, a one-way valve is formed by an area of damaged tissue, and the amount of air in the space between chest wall and lungs increases; this is called a tension pneumothorax. This can cause a steadily worsening oxygen shortage and low blood pressure. This leads to a type of shock called obstructive shock, which can be fatal unless reversed. Very rarely, both lungs may be affected by a pneumothorax. It is often called a "collapsed lung", although that term may also refer to atelectasis.

In human anatomy, the thoracic duct is the larger of the two lymph ducts of the lymphatic system. The thoracic duct usually begins from the upper aspect of the cisterna chyli, passing out of the abdomen through the aortic hiatus into first the posterior mediastinum and then the superior mediastinum, extending as high up as the root of the neck before descending to drain into the systemic (blood) circulation at the venous angle.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. This equals to 9–20 cmH2O, which is a common scale used in lumbar punctures. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.
Kussmaul's sign is a paradoxical rise in jugular venous pressure (JVP) on inspiration, or a failure in the appropriate fall of the JVP with inspiration. It can be seen in some forms of heart disease and is usually indicative of limited right ventricular filling due to right heart dysfunction.

The jugular venous pressure is the indirectly observed pressure over the venous system via visualization of the internal jugular vein. It can be useful in the differentiation of different forms of heart and lung disease. Classically three upward deflections and two downward deflections have been described.

The jugular veins are veins that take blood from the head back to the heart via the superior vena cava. The internal jugular vein descends next to the internal carotid artery and continues posteriorly to the sternocleidomastoid muscle.
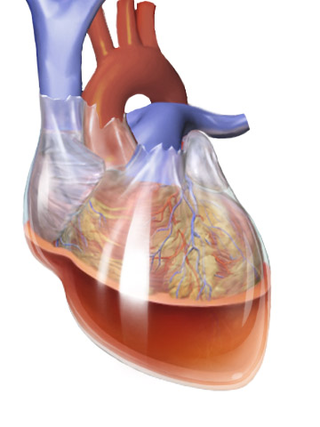
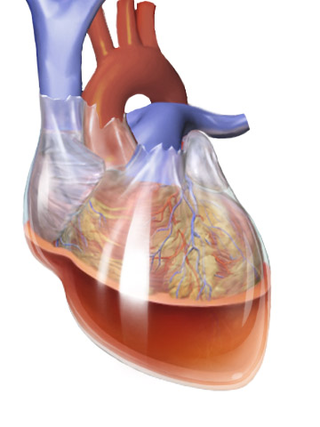
Beck's triad is a collection of three medical signs associated with acute cardiac tamponade, a medical emergency when excessive fluid accumulates in the pericardial sac around the heart and impairs its ability to pump blood. The signs are low arterial blood pressure, distended neck veins, and distant, muffled heart sounds.
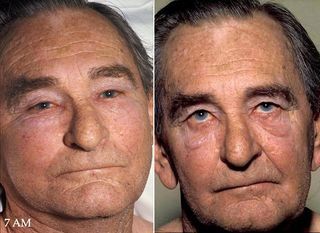
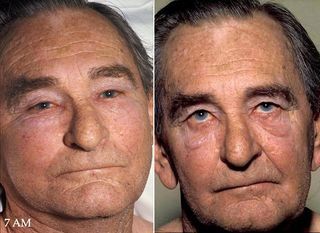
Superior vena cava syndrome (SVCS), is a group of symptoms caused by obstruction of the superior vena cava ("SVC"), a short, wide vessel carrying circulating blood into the heart. The majority of cases are caused by malignant tumors within the mediastinum, most commonly lung cancer and non-Hodgkin's lymphoma, directly compressing or invading the SVC wall. Non-malignant causes are increasing in prevalence due to expanding use of intravascular devices, which can result in thrombosis. Other non-malignant causes include benign mediastinal tumors, aortic aneurysm, infections, and fibrosing mediastinitis.

A hemothorax is an accumulation of blood within the pleural cavity. The symptoms of a hemothorax may include chest pain and difficulty breathing, while the clinical signs may include reduced breath sounds on the affected side and a rapid heart rate. Hemothoraces are usually caused by an injury, but they may occur spontaneously due to cancer invading the pleural cavity, as a result of a blood clotting disorder, as an unusual manifestation of endometriosis, in response to pneumothorax, or rarely in association with other conditions.

The subclavian vein is a paired large vein, one on either side of the body, that is responsible for draining blood from the upper extremities, allowing this blood to return to the heart. The left subclavian vein plays a key role in the absorption of lipids, by allowing products that have been carried by lymph in the thoracic duct to enter the bloodstream. The diameter of the subclavian veins is approximately 1–2 cm, depending on the individual.

A chylothorax is an abnormal accumulation of chyle, a type of lipid-rich lymph, in the space surrounding the lung. The lymphatics of the digestive system normally returns lipids absorbed from the small bowel via the thoracic duct, which ascends behind the esophagus to drain into the left brachiocephalic vein. If normal thoracic duct drainage is disrupted, either due to obstruction or rupture, chyle can leak and accumulate within the negative-pressured pleural space. In people on a normal diet, this fluid collection can sometimes be identified by its turbid, milky white appearance, since chyle contains emulsified triglycerides.
The abdominojugular test, also known as abdominojugular reflux (AJR), is a physical examination test useful in diagnosing right ventricle dysfunction, particularly right ventricular failure.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, describes a physical trauma due to a forceful impact without penetration of the body's surface. Blunt trauma stands in contrast with penetrating trauma, which occurs when an object pierces the skin, enters body tissue, and creates an open wound. Blunt trauma occurs due to direct physical trauma or impactful force to a body part. Such incidents often occur with road traffic collisions, assaults, and sports-related injuries, and are notably common among the elderly who experience falls.

Pneumomediastinum is pneumatosis in the mediastinum, the central part of the chest cavity. First described in 1819 by René Laennec, the condition can result from physical trauma or other situations that lead to air escaping from the lungs, airways, or bowel into the chest cavity. In underwater divers it is usually the result of pulmonary barotrauma.

The bronchomediastinal lymph trunks are essential components of the human lymphatic system, tasked with draining lymph from the tracheobronchial, internal mammary, and anterior mediastinal lymph nodes.

A pulmonary contusion, also known as lung contusion, is a bruise of the lung, caused by chest trauma. As a result of damage to capillaries, blood and other fluids accumulate in the lung tissue. The excess fluid interferes with gas exchange, potentially leading to inadequate oxygen levels (hypoxia). Unlike pulmonary laceration, another type of lung injury, pulmonary contusion does not involve a cut or tear of the lung tissue.

A pulmonary laceration is a chest injury in which lung tissue is torn or cut. An injury that is potentially more serious than pulmonary contusion, pulmonary laceration involves disruption of the architecture of the lung, while pulmonary contusion does not. Pulmonary laceration is commonly caused by penetrating trauma but may also result from forces involved in blunt trauma such as shear stress. A cavity filled with blood, air, or both can form. The injury is diagnosed when collections of air or fluid are found on a CT scan of the chest. Surgery may be required to stitch the laceration, to drain blood, or even to remove injured parts of the lung. The injury commonly heals quickly with few problems if it is given proper treatment; however it may be associated with scarring of the lung or other complications.
Obstructive shock is one of the four types of shock, caused by a physical obstruction in the flow of blood. Obstruction can occur at the level of the great vessels or the heart itself. Causes include pulmonary embolism, cardiac tamponade, and tension pneumothorax. These are all life-threatening. Symptoms may include shortness of breath, weakness, or altered mental status. Low blood pressure and tachycardia are often seen in shock. Other symptoms depend on the underlying cause.
The Hs and Ts is a mnemonic used to aid in remembering the possible reversible causes of cardiac arrest. A variety of disease processes can lead to a cardiac arrest; however, they usually boil down to one or more of the "Hs and Ts".