A febrile seizure, also known as a fever fit or febrile convulsion, is a seizure associated with a high body temperature but without any serious underlying health issue. They most commonly occur in children between the ages of 6 months and 5 years. Most seizures are less than five minutes in duration, and the child is completely back to normal within an hour of the event. There are two types: simple febrile seizures and complex febrile seizures. Simple febrile seizures involve an otherwise healthy child who has at most one tonic-clonic seizure lasting less than 15 minutes in a 24-hour period. Complex febrile seizures have focal symptoms, last longer than 15 minutes, or occur more than once within 24 hours. About 80% are classified as simple febrile seizures.
This is a timeline of the development of prophylactic human vaccines. Early vaccines may be listed by the first year of development or testing, but later entries usually show the year the vaccine finished trials and became available on the market. Although vaccines exist for the diseases listed below, only smallpox has been eliminated worldwide. The other vaccine-preventable illnesses continue to cause millions of deaths each year. Currently, polio and measles are the targets of active worldwide eradication campaigns.
ATC code J07Vaccines is a therapeutic subgroup of the Anatomical Therapeutic Chemical Classification System, a system of alphanumeric codes developed by the World Health Organization (WHO) for the classification of drugs and other medical products. Subgroup J07 is part of the anatomical group J Antiinfectives for systemic use.

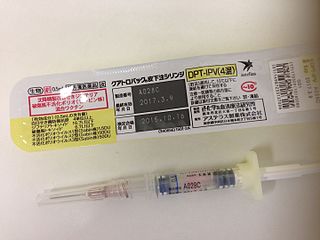
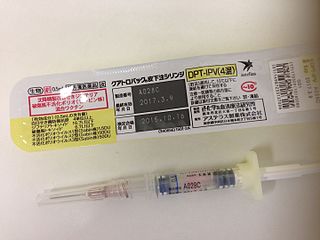
The DPT vaccine or DTP vaccine is a class of combination vaccines against three infectious diseases in humans: diphtheria, pertussis, and tetanus (lockjaw). The vaccine components include diphtheria and tetanus toxoids, and either killed whole cells of the bacterium that causes pertussis or pertussis antigens. The term toxoid refers to vaccines which use an inactivated toxin produced by the pathogen which they are targeted against to generate an immune response. In this way, the toxoid vaccine generates an immune response which is targeted against the toxin which is produced by the pathogen and causes disease, rather than a vaccine which is targeted against the pathogen itself. The whole cells or antigens will be depicted as either "DTwP" or "DTaP", where the lower-case "w" indicates whole-cell inactivated pertussis and the lower-case "a" stands for "acellular". In comparison to alternative vaccine types, such as live attenuated vaccines, the DTP vaccine does not contain any live pathogen, but rather uses inactivated toxoid to generate an immune response; therefore, there is not a risk of use in populations that are immune compromised since there is not any known risk of causing the disease itself. As a result, the DTP vaccine is considered a safe vaccine to use in anyone and it generates a much more targeted immune response specific for the pathogen of interest.

The schedule for childhood immunizations in the United States is published by the Centers for Disease Control and Prevention (CDC). The vaccination schedule is broken down by age: birth to six years of age, seven to eighteen, and adults nineteen and older. Childhood immunizations are key in preventing diseases with epidemic potential.
Immunization during pregnancy is the administration of a vaccine to a pregnant individual. This may be done either to protect the individual from disease or to induce an antibody response, such that the antibodies cross the placenta and provide passive immunity to the infant after birth. In many countries, including the US, Canada, UK, Australia and New Zealand, vaccination against influenza, COVID-19 and whooping cough is routinely offered during pregnancy.

The Haemophilus influenzae type B vaccine, also known as Hib vaccine, is a vaccine used to prevent Haemophilus influenzae type b (Hib) infection. In countries that include it as a routine vaccine, rates of severe Hib infections have decreased more than 90%. It has therefore resulted in a decrease in the rate of meningitis, pneumonia, and epiglottitis.
The Expanded Program on Immunization is a World Health Organization program with the goal to make vaccines available to all children.
Tetanus vaccine, also known as tetanus toxoid (TT), is a toxoid vaccine used to prevent tetanus. During childhood, five doses are recommended, with a sixth given during adolescence.
Universal Immunisation Programme (UIP) is a vaccination programme launched by the Government of India in 1985. It became a part of Child Survival and Safe Motherhood Programme in 1992 and is currently one of the key areas under the National Health Mission since 2005. The programme now consists of vaccination for 12 diseases- tuberculosis, diphtheria, pertussis, tetanus, poliomyelitis, measles, hepatitis B, rotaviral gastroenteritis, Japanese encephalitis, rubella, pneumonia and Pneumococcal diseases. Hepatitis B and Pneumococcal diseases were added to the UIP in 2007 and 2017 respectively. The cost of all the vaccines are borne entirely by the Government of India and is funded through taxes with a budget of ₹7,234 crore (US$870 million) in 2022 and the program covers all residents of India, including foreign residents.
The Vaccine Damage Payment is a provision of the welfare state in the United Kingdom that provides a payment of £120,000, as of 2023, for people who can show that they have suffered a vaccine injury.
The Norwegian Institute of Public Health is responsible for maintaining and revising the list of notifiable diseases in Norway and participates in the European Centre for Disease Prevention and Control (ECDC) and the World Health Organization's surveillance of infectious diseases. The notifiable diseases are classified into Group A, Group B and Group C diseases, depending on the procedure for reporting the disease.
In the United States, the National Notifiable Disease Surveillance System (NNDSS) is responsible for sharing information regarding notifiable diseases. As of 2020, the following are the notifiable diseases in the US as mandated by the Centers for Disease Control and Prevention:
DTaP-IPV/Hib vaccine is a 5-in-1 combination vaccine that protects against diphtheria, tetanus, whooping cough, polio, and Haemophilus influenzae type B.
DTaP-IPV-HepB vaccine is a combination vaccine whose generic name is diphtheria and tetanus toxoids and acellular pertussis adsorbed, hepatitis B (recombinant) and inactivated polio vaccine or DTaP-IPV-Hep B. It protects against the infectious diseases diphtheria, tetanus, pertussis, poliomyelitis, and hepatitis B.

A hexavalent vaccine, or 6-in-1 vaccine, is a combination vaccine with six individual vaccines conjugated into one, intended to protect people from multiple diseases. The term usually refers to the children's vaccine that protects against diphtheria, tetanus, pertussis, poliomyelitis, haemophilus B, and hepatitis B, which is used in more than 90 countries around the world including in Europe, Canada, Australia, Jordan, and New Zealand.
A notifiable disease is one which the law requires to be reported to government authorities.

The Australian National Immunisation Program Schedule sets out the immunisations Australians are given at different stages in their life. The program aims to reduce the number of preventable disease cases in Australia by increasing national immunisation coverage. The program starts for an Australian when they are born. Vaccinations are given at birth, then again when the baby is 2 months, 4 months, 6 months, 12 months and 18 months. The immunisation schedule continues when the child is 4 years old, and then into adolescent years. The program is not compulsory and parents have the choice if they want their child vaccinated.