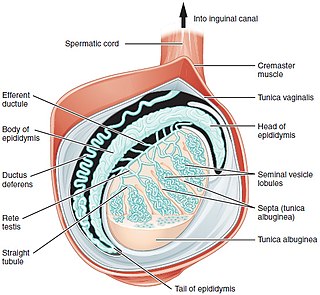
A testicle or testis is the male gonad in all bilaterians, including humans. It is homologous to the female ovary. The functions of the testicles are to produce both sperm and androgens, primarily testosterone. Testosterone release is controlled by the anterior pituitary luteinizing hormone, whereas sperm production is controlled both by the anterior pituitary follicle-stimulating hormone and gonadal testosterone.
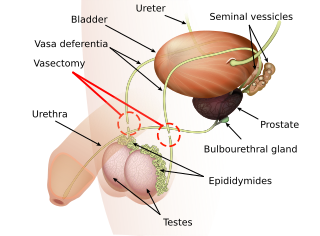
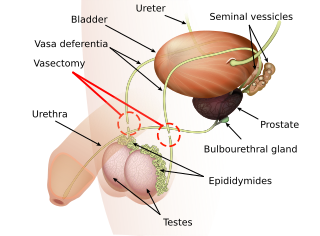
Vasectomy is an elective surgical procedure that results in male sterilization, often as a means of permanent contraception. During the procedure, the male vasa deferentia are cut and tied or sealed so as to prevent sperm from entering into the urethra and thereby prevent fertilization of a female through sexual intercourse. Vasectomies are usually performed in a physician's office, medical clinic, or, when performed on a non-human animal, in a veterinary clinic. Hospitalization is not normally required as the procedure is not complicated, the incisions are small, and the necessary equipment routine.
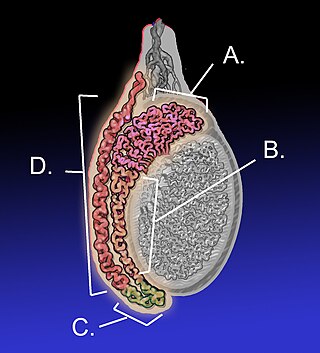
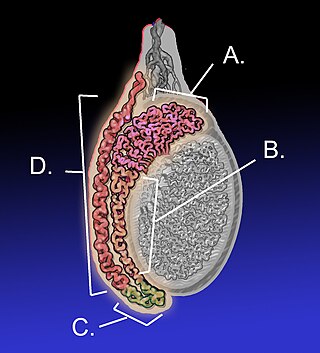
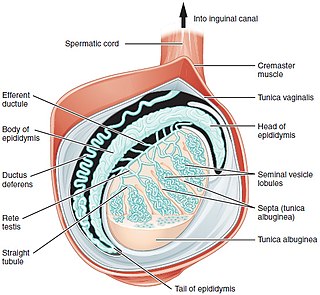
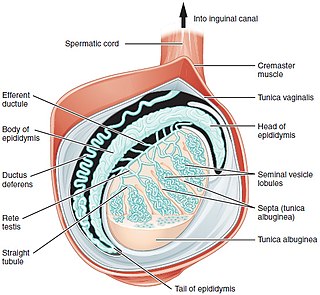
The epididymis is an elongated tubular structure attached to the posterior side of each one of the two male reproductive glands, the testicles. It is a single, narrow, tightly coiled tube in adult humans, 6 to 7 centimetres in length; uncoiled the tube would be approximately 6 m long. It connects the testicle to the vas deferens in the male reproductive system. The epididymis serves as an interconnection between the multiple efferent ducts at the rear of a testicle (proximally), and the vas deferens (distally). Its primary function is the storage, maturation and transport of sperm cells.

The vas deferens, with the more modern name ductus deferens, is part of the male reproductive system of many vertebrates. The ducts transport sperm from the epididymides to the ejaculatory ducts in anticipation of ejaculation. The vas deferens is a partially coiled tube which exits the abdominal cavity through the inguinal canal.

Spermatogenesis is the process by which haploid spermatozoa develop from germ cells in the seminiferous tubules of the testicle. This process starts with the mitotic division of the stem cells located close to the basement membrane of the tubules. These cells are called spermatogonial stem cells. The mitotic division of these produces two types of cells. Type A cells replenish the stem cells, and type B cells differentiate into primary spermatocytes. The primary spermatocyte divides meiotically into two secondary spermatocytes; each secondary spermatocyte divides into two equal haploid spermatids by Meiosis II. The spermatids are transformed into spermatozoa (sperm) by the process of spermiogenesis. These develop into mature spermatozoa, also known as sperm cells. Thus, the primary spermatocyte gives rise to two cells, the secondary spermatocytes, and the two secondary spermatocytes by their subdivision produce four spermatozoa and four haploid cells.

Persistent Müllerian duct syndrome (PMDS) is the presence of Müllerian duct derivatives in what would be considered a genetically and otherwise physically normal male animal by typical human based standards. In humans, PMDS typically is due to an autosomal recessive congenital disorder and is considered by some to be a form of pseudohermaphroditism due to the presence of Müllerian derivatives. PMDS can also present in non-human animals.
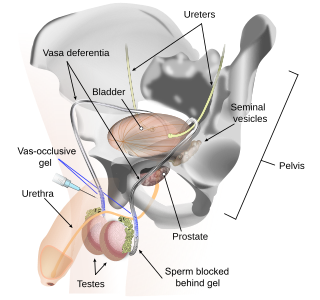
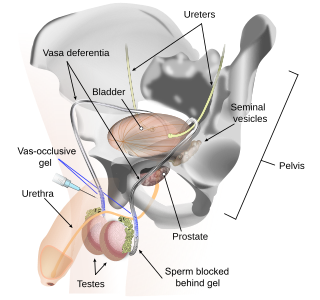
Vas-occlusive contraception is a form of male contraception that blocks sperm transport in the vas deferens, the tubes that carry sperm from the epididymis to the ejaculatory ducts.

Azoospermia is the medical condition of a man whose semen contains no sperm. It is associated with male infertility, but many forms are amenable to medical treatment. In humans, azoospermia affects about 1% of the male population and may be seen in up to 20% of male infertility situations in Canada.
Male contraceptives, also known as male birth control, are methods of preventing pregnancy by interrupting the function of sperm. The main forms of male contraception available today are condoms, vasectomy, and withdrawal, which together represented 20% of global contraceptive use in 2019. New forms of male contraception are in clinical and preclinical stages of research and development, but as of 2024, none have reached regulatory approval for widespread use.
Terms oligospermia, oligozoospermia, and low sperm count refer to semen with a low concentration of sperm and is a common finding in male infertility. Often semen with a decreased sperm concentration may also show significant abnormalities in sperm morphology and motility. There has been interest in replacing the descriptive terms used in semen analysis with more quantitative information.
Hypospermia is a condition in which a man has an unusually low ejaculate volume, less than 1.5 mL. It is the opposite of hyperspermia, which is a semen volume of more than 5.5 mL. It should not be confused with oligospermia, which means low sperm count. Normal ejaculate when a man is not drained from prior sex and is suitably aroused is around 1.5–6 mL, although this varies greatly with mood, physical condition, and sexual activity. Of this, around 1% by volume is sperm cells. The U.S.-based National Institutes of Health defines hypospermia as a semen volume lower than 2 mL on at least two semen analyses.
Male infertility refers to a sexually mature male's inability to impregnate a fertile female. In humans, it accounts for 40–50% of infertility. It affects approximately 7% of all men. Male infertility is commonly due to deficiencies in the semen, and semen quality is used as a surrogate measure of male fecundity. More recently, advance sperm analyses that examine intracellular sperm components are being developed.
Testicular sperm extraction (TESE) is a surgical procedure in which a small portion of tissue is removed from the testicle and any viable sperm cells from that tissue are extracted for use in further procedures, most commonly intracytoplasmic sperm injection (ICSI) as part of in vitro fertilisation (IVF). TESE is often recommended to patients who cannot produce sperm by ejaculation due to azoospermia.
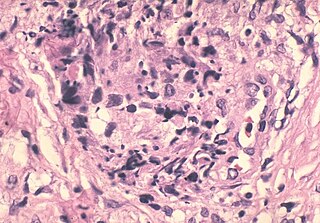
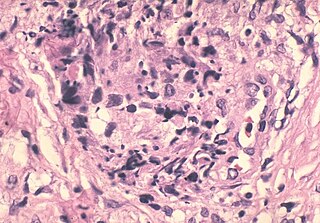
A sperm granuloma is a lump of leaked sperm that appears along the vasa deferentia or epididymides in vasectomized individuals. While the majority of sperm granulomas are present along the vas deferens, the rest of them form at the epididymis. Sperm granulomas range in size, from one millimeter to one centimeter. They consist of a central mass of degenerating sperm surrounded by tissue containing blood vessels and immune system cells. Sperm granulomas may also have a yellow, white, or cream colored center when cut open. While some sperm granulomas can be painful, most of them are painless and asymptomatic. Sperm granulomas can appear as a result of surgery, trauma, or an infection. They can appear as early as four days after surgery and fully formed ones can appear as late as 208 days later.
Vasectomy reversal is a term used for surgical procedures that reconnect the male reproductive tract after interruption by a vasectomy. Two procedures are possible at the time of vasectomy reversal: vasovasostomy and vasoepididymostomy. Although vasectomy is considered a permanent form of contraception, advances in microsurgery have improved the success of vasectomy reversal procedures. The procedures remain technically demanding and may not restore the pre-vasectomy condition.
FNA mapping is an application of fine-needle aspiration (FNA) to the testis for the diagnosis of male infertility. FNA cytology has been used to examine pathological human tissue from various organs for over 100 years. As an alternative to open testicular biopsy for the last 40 years, FNA mapping has helped to characterize states of human male infertility due to defective spermatogenesis. Although recognized as a reliable, and informative technique, testis FNA has not been widely used in U.S. to evaluate male infertility. Recently, however, testicular FNA has gained popularity as both a diagnostic and therapeutic tool for the management of clinical male infertility for several reasons:
- The testis is an ideal organ for evaluation by FNA because of its uniform cellularity and easy accessibility.
- The trend toward minimally invasive procedures and cost-containment views FNA favorably compared to surgical testis biopsy.
- The realization that the specific histologic abnormality observed on testis biopsy has no definite correlation to either the etiology of infertility or to the ability to find sperm for assisted reproduction.
- Assisted reproduction has undergone dramatic advances such that testis sperm are routinely used for biological pregnancies, thus fueling the development of novel FNA techniques to both locate and procure sperm.

Dr. Paul J Turek is an American physician and surgeon, men's reproductive health specialist, and businessman. Turek is a recent recipient of a National Institutes of Health (NIH) grant for research designed to help infertile men become fathers using stem cells.
Vasoepididymostomy or epididymovasostomy is a surgery by which vasectomies are reversed. It involves connection of the severed vas deferens to the epididymis and is more technically demanding than the vasovasostomy.

Male accessory gland infection (MAGI) is a condition with signs of inflammation involving one or more sites in the male genital tract. Diagnosis is made according to parameters defined by the World Health Organization, and it is particularly made in relation to infectious or inflammatory causes of male infertility.
Cryopreservation of testicular tissue is an experimental method being used to preserve fertility in pre-pubescent males, or males who cannot produce sperm, to allow them the option of having biological children.