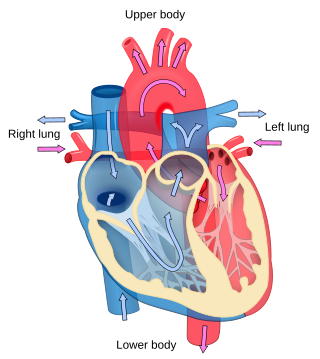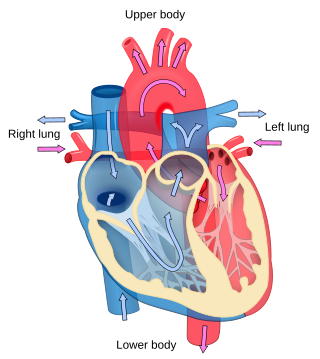
Cardiology is the study of the heart. Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease, and electrophysiology. Physicians who specialize in this field of medicine are called cardiologists, a specialty of internal medicine. Pediatric cardiologists are pediatricians who specialize in cardiology. Physicians who specialize in cardiac surgery are called cardiothoracic surgeons or cardiac surgeons, a specialty of general surgery.

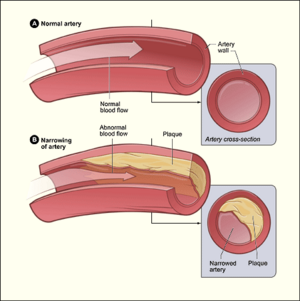
Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of atherosclerotic plaque in the arteries of the heart. It is the most common of the cardiovascular diseases. Types include stable angina, unstable angina, and myocardial infarction. A common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw. Occasionally it may feel like heartburn. Usually symptoms occur with exercise or emotional stress, last less than a few minutes, and improve with rest. Shortness of breath may also occur and sometimes no symptoms are present. In many cases, the first sign is a heart attack. Other complications include heart failure or an abnormal heartbeat.

Cardiomyopathy is a group of primary diseases of the heart muscle. Early on there may be few or no symptoms. As the disease worsens, shortness of breath, feeling tired, and swelling of the legs may occur, due to the onset of heart failure. An irregular heart beat and fainting may occur. Those affected are at an increased risk of sudden cardiac death.

Angina, also known as angina pectoris, is chest pain or pressure, usually caused by insufficient blood flow to the heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.

Coronary artery bypass surgery, also known as coronary artery bypass graft, is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pain caused by CAD, slow the progression of CAD, and increase life expectancy. It aims to bypass narrowings in heart arteries by using arteries or veins harvested from other parts of the body, thus restoring adequate blood supply to the previously ischemic heart.
An ejection fraction (EF) is the volumetric fraction of fluid ejected from a chamber with each contraction. It can refer to the cardiac atrium, ventricle, gall bladder, or leg veins, although if unspecified it usually refers to the left ventricle of the heart. EF is widely used as a measure of the pumping efficiency of the heart and is used to classify heart failure types. It is also used as an indicator of the severity of heart failure, although it has recognized limitations.

Hypertensive heart disease includes a number of complications of high blood pressure that affect the heart. While there are several definitions of hypertensive heart disease in the medical literature, the term is most widely used in the context of the International Classification of Diseases (ICD) coding categories. The definition includes heart failure and other cardiac complications of hypertension when a causal relationship between the heart disease and hypertension is stated or implied on the death certificate. In 2013 hypertensive heart disease resulted in 1.07 million deaths as compared with 630,000 deaths in 1990.

Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the insertion of a permanent wire-meshed tube that is either drug eluting (DES) or composed of bare metal (BMS). The stent delivery balloon from the angioplasty catheter is inflated with media to force contact between the struts of the stent and the vessel wall, thus widening the blood vessel diameter. After accessing the blood stream through the femoral or radial artery, the procedure uses coronary catheterization to visualise the blood vessels on X-ray imaging. After this, an interventional cardiologist can perform a coronary angioplasty, using a balloon catheter in which a deflated balloon is advanced into the obstructed artery and inflated to relieve the narrowing; certain devices such as stents can be deployed to keep the blood vessel open.
Myocardial stunning or transient post-ischemic myocardial dysfunction is a state of mechanical cardiac dysfunction that can occur in a portion of myocardium without necrosis after a brief interruption in perfusion, despite the timely restoration of normal coronary blood flow. In this situation, even after ischemia has been relieved and myocardial blood flow (MBF) returns to normal, myocardial function is still depressed for a variable period of time, usually days to weeks. This reversible reduction of function of heart contraction after reperfusion is not accounted for by tissue damage or reduced blood flow, but rather, its thought to represent a perfusion-contraction "mismatch". Myocardial stunning was first described in laboratory canine experiments in the 1970s where LV wall abnormalities were observed following coronary artery occlusion and subsequent reperfusion.

Takotsubo cardiomyopathy or takotsubo syndrome (TTS), also known as stress cardiomyopathy, is a type of non-ischemic cardiomyopathy in which there is a sudden temporary weakening of the muscular portion of the heart. It usually appears after a significant stressor, either physical or emotional; when caused by the latter, the condition is sometimes called broken heart syndrome. Examples of physical stressors that can cause TTS are sepsis, shock, subarachnoid hemorrhage, and pheochromocytoma. Emotional stressors include bereavement, divorce, or the loss of a job. Reviews suggest that of patients diagnosed with the condition, about 70–80% recently experienced a major stressor, including 41–50% with a physical stressor and 26–30% with an emotional stressor. TTS can also appear in patients who have not experienced major stressors.

Myocardial perfusion imaging or scanning is a nuclear medicine procedure that illustrates the function of the heart muscle (myocardium).

Noncompaction cardiomyopathy (NCC) is a rare congenital disease of heart muscle that affects both children and adults. It results from abnormal prenatal development of heart muscle.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.

Coronary ischemia, myocardial ischemia, or cardiac ischemia, is a medical term for a reduced blood flow in the coronary circulation through the coronary arteries. Coronary ischemia is linked to heart disease, and heart attacks. Coronary arteries deliver oxygen-rich blood to the heart muscle. Reduced blood flow to the heart associated with coronary ischemia can result in inadequate oxygen supply to the heart muscle. When oxygen supply to the heart is unable to keep up with oxygen demand from the muscle, the result is the characteristic symptoms of coronary ischemia, the most common of which is chest pain. Chest pain due to coronary ischemia commonly radiates to the arm or neck. Certain individuals such as women, diabetics, and the elderly may present with more varied symptoms. If blood flow through the coronary arteries is stopped completely, cardiac muscle cells may die, known as a myocardial infarction, or heart attack.

A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat, feeling tired, and decreased level of consciousness. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest.

Coronary perfusion pressure (CPP) refers to the pressure gradient that drives coronary blood pressure. The heart's function is to perfuse blood to the body; however, the heart's own myocardium must, itself, be supplied for its own muscle function. The heart is supplied by coronary vessels, and therefore CPP is the blood pressure within those vessels. If pressures are too low in the coronary vasculature, then the myocardium risks ischemia with subsequent myocardial infarction or cardiogenic shock.

Reperfusion therapy is a medical treatment to restore blood flow, either through or around, blocked arteries, typically after a heart attack. Reperfusion therapy includes drugs and surgery. The drugs are thrombolytics and fibrinolytics used in a process called thrombolysis. Surgeries performed may be minimally-invasive endovascular procedures such as a percutaneous coronary intervention (PCI), which involves coronary angioplasty. The angioplasty uses the insertion of a balloon and/or stents to open up the artery. Other surgeries performed are the more invasive bypass surgeries that graft arteries around blockages.
A diagnosis of myocardial infarction is created by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers. A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.
Remote ischemic conditioning (RIC) is an experimental medical procedure that aims to reduce the severity of ischaemic injury to an organ such as the heart or the brain, most commonly in the situation of a heart attack or a stroke, or during procedures such as heart surgery when the heart may temporary suffer ischaemia during the operation, by triggering the body's natural protection against tissue injury. Although noted to have some benefits in experimental models in animals, this is still an experimental procedure in humans and initial evidence from small studies have not been replicated in larger clinical trials. Successive clinical trials have failed to identify evidence supporting a protective role in humans.

Roberto Ferrari is an Italian cardiologist who currently holds the position of Emeritus Professor at the University of Ferrara, where besides he was the chair of the Cardiology in the School of Medicine until the 2019–2020 academic year.