Related Research Articles
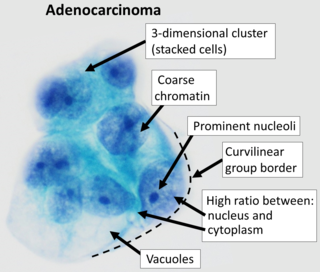
Adenocarcinoma is a type of cancerous tumor that can occur in several parts of the body. It is defined as neoplasia of epithelial tissue that has glandular origin, glandular characteristics, or both. Adenocarcinomas are part of the larger grouping of carcinomas, but are also sometimes called by more precise terms omitting the word, where these exist. Thus invasive ductal carcinoma, the most common form of breast cancer, is adenocarcinoma but does not use the term in its name—however, esophageal adenocarcinoma does to distinguish it from the other common type of esophageal cancer, esophageal squamous cell carcinoma. Several of the most common forms of cancer are adenocarcinomas, and the various sorts of adenocarcinoma vary greatly in all their aspects, so that few useful generalizations can be made about them.

Carcinoma is a malignancy that develops from epithelial cells. Specifically, a carcinoma is a cancer that begins in a tissue that lines the inner or outer surfaces of the body, and that arises from cells originating in the endodermal, mesodermal or ectodermal germ layer during embryogenesis.

A serous tumour is a neoplasm that typically has papillary to solid formations of tumor cells with crowded nuclei, and which typically arises on the modified Mullerian-derived serous membranes that surround the ovaries in females. Such ovarian tumors are part of the surface epithelial-stromal tumour group of ovarian tumors. They are common neoplasms with a strong tendency to occur bilaterally, and they account for approximately a quarter of all ovarian tumors.

Surface epithelial-stromal tumors are a class of ovarian neoplasms that may be benign or malignant. Neoplasms in this group are thought to be derived from the ovarian surface epithelium or from ectopic endometrial or Fallopian tube (tubal) tissue. Tumors of this type are also called ovarian adenocarcinoma. This group of tumors accounts for 90% to 95% of all cases of ovarian cancer; however is mainly only found in postmenopausal women with the exception of the United States where 7% of cases occur in women under the age of 40. Serum CA-125 is often elevated but is only 50% accurate so it is not a useful tumor marker to assess the progress of treatment. 75% of women with epithelial ovarian cancer are found within the advanced-stages; however younger patients are more likely to have better prognoses than older patients.

Pseudomyxoma peritonei (PMP) is a clinical condition caused by cancerous cells that produce abundant mucin or gelatinous ascites. The tumors cause fibrosis of tissues and impede digestion or organ function, and if left untreated, the tumors and mucin they produce will fill the abdominal cavity. This will result in compression of organs and will destroy the function of the colon, small intestine, stomach, or other organs. Prognosis with treatment in many cases is optimistic, but the disease is lethal if untreated, with death occurring via cachexia, bowel obstruction, or other types of complications.

Adenocarcinoma in situ (AIS) of the lung —previously included in the category of "bronchioloalveolar carcinoma" (BAC)—is a subtype of lung adenocarcinoma. It tends to arise in the distal bronchioles or alveoli and is defined by a non-invasive growth pattern. This small solitary tumor exhibits pure alveolar distribution and lacks any invasion of the surrounding normal lung. If completely removed by surgery, the prognosis is excellent with up to 100% 5-year survival.

Cystadenocarcinoma is a malignant form of a cystadenoma and is a cancer derived from glandular epithelium, in which cystic accumulations of retained secretions are formed. The neoplastic cells manifest varying degrees of anaplasia and invasiveness, and local extension and metastases occur. Cystadenocarcinomas develop frequently in the ovaries, where pseudomucinous and serous types are recognized. Similar tumor histology has also been reported in the pancreas, although it is a considerably rarer entity representing 1–1.5% of all Pancreatic cancer.
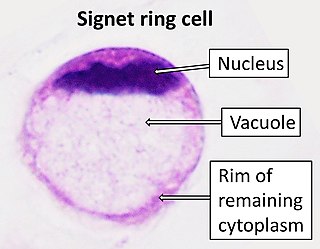
Signet ring cell carcinoma (SRCC) is a rare form of highly malignant adenocarcinoma that produces mucin. It is an epithelial malignancy characterized by the histologic appearance of signet ring cells.

A mucinous neoplasm is an abnormal and excessive growth of tissue (neoplasia) with associated mucin. It arises from epithelial cells that line certain internal organs and skin, and produce mucin. A malignant mucinous neoplasm is called a mucinous carcinoma. For example, for ovarian mucinous tumors, approximately 75% are benign, 10% are borderline and 15% are malignant.

Mucinous cystadenoma is a benign cystic tumor lined by a mucinous epithelium. It is a type of cystic adenoma (cystadenoma).

Intraductal papillary mucinous neoplasm (IPMN) is a type of tumor that can occur within the cells of the pancreatic duct. IPMN tumors produce mucus, and this mucus can form pancreatic cysts. Although intraductal papillary mucinous neoplasms are benign tumors, they can progress to pancreatic cancer. As such IPMN is viewed as a precancerous condition. Once an intraductal papillary mucinous neoplasm has been found, the management options include close monitoring and pre-emptive surgery.

Fetal adenocarcinoma (FA) of the lung is a rare subtype of pulmonary adenocarcinoma that exhibits tissue architecture and cell characteristics that resemble fetal lung tissue upon microscopic examination. It is currently considered a variant of solid adenocarcinoma with mucin production.
Large cell lung carcinoma with rhabdoid phenotype (LCLC-RP) is a rare histological form of lung cancer, currently classified as a variant of large cell lung carcinoma (LCLC). In order for a LCLC to be subclassified as the rhabdoid phenotype variant, at least 10% of the malignant tumor cells must contain distinctive structures composed of tangled intermediate filaments that displace the cell nucleus outward toward the cell membrane. The whorled eosinophilic inclusions in LCLC-RP cells give it a microscopic resemblance to malignant cells found in rhabdomyosarcoma (RMS), a rare neoplasm arising from transformed skeletal muscle. Despite their microscopic similarities, LCLC-RP is not associated with rhabdomyosarcoma.
Epithelial-myoepithelial carcinoma of the lung is a very rare histologic form of malignant epithelial neoplasm ("carcinoma") arising from lung tissue.

Adenocarcinoma of the lung is the most common type of lung cancer, and like other forms of lung cancer, it is characterized by distinct cellular and molecular features. It is classified as one of several non-small cell lung cancers (NSCLC), to distinguish it from small cell lung cancer which has a different behavior and prognosis. Lung adenocarcinoma is further classified into several subtypes and variants. The signs and symptoms of this specific type of lung cancer are similar to other forms of lung cancer, and patients most commonly complain of persistent cough and shortness of breath.
Acinar adenocarcinoma is a histological subtype of gland-forming cancer that is diagnosed when cuboidal and/or columnar shaped malignant cells in the neoplastic tissue form acini and tubules. It is a common form of cancer occurring in the lung and prostate gland.
Sarcomatoid carcinoma of the lung is a term that encompasses five distinct histological subtypes of lung cancer, including (1) pleomorphic carcinoma, (2) spindle cell carcinoma, (3) giant cell carcinoma, (4) carcinosarcoma, or (5) pulmonary blastoma.

Giant-cell carcinoma of the lung (GCCL) is a rare histological form of large-cell lung carcinoma, a subtype of undifferentiated lung cancer, traditionally classified within the non-small-cell lung carcinomas (NSCLC).

Ceruminous adenocarcinoma is a malignant neoplasm derived from ceruminous glands of the external auditory canal. This tumor is rare, with several names used in the past. Synonyms have included cylindroma, ceruminoma, ceruminous adenocarcinoma, not otherwise specified (NOS), ceruminous adenoid cystic carcinoma (ACC), and ceruminous mucoepidermoid carcinoma.
Pulmonary enteric adenocarcinoma is rare subtype of pulmonary adenocarcinoma.
References
- 1 2 3 4 5 6 7 8 9 Gao ZH, Urbanski SJ (July 2005). "The spectrum of pulmonary mucinous cystic neoplasia : a clinicopathologic and immunohistochemical study of ten cases and review of literature". American Journal of Clinical Pathology. 124 (1): 62–70. doi: 10.1309/52XXR6E6U0J2JX0F . PMID 15923171.
- 1 2 3 Travis, William D; Brambilla, Elisabeth; Muller-Hermelink, H Konrad; et al., eds. (2004). Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart (PDF). World Health Organization Classification of Tumours. Lyon: IARC Press. ISBN 978-92-832-2418-1. Archived from the original (PDF) on 23 August 2009. Retrieved 27 March 2010.
- ↑ Tsuta K, Ishii G, Nitadori J, Murata Y, Kodama T, Nagai K, Ochiai A (May 2006). "Comparison of the immunophenotypes of signet-ring cell carcinoma, solid adenocarcinoma with mucin production, and mucinous bronchioloalveolar carcinoma of the lung characterized by the presence of cytoplasmic mucin". The Journal of Pathology. 209 (1): 78–87. doi:10.1002/path.1947. PMID 16463270. S2CID 22202641.
- 1 2 3 Tangthangtham A, Chonmaitri I, Tungsagunwattana S, Charupatanapongse U (October 1998). "Mucinous cystadenocarcinoma of the lung". Journal of the Medical Association of Thailand = Chotmaihet Thangphaet. 81 (10): 794–798. PMID 9803072.
- ↑ Kragel PJ, Devaney KO, Meth BM, Linnoila I, Frierson HF, Travis WD (October 1990). "Mucinous cystadenoma of the lung. A report of two cases with immunohistochemical and ultrastructural analysis". Archives of Pathology & Laboratory Medicine. 114 (10): 1053–1056. PMID 1699507.
- ↑ Dixon AY, Moran JF, Wesselius LJ, McGregor DH (July 1993). "Pulmonary mucinous cystic tumor. Case report with review of the literature". The American Journal of Surgical Pathology. 17 (7): 722–728. doi:10.1097/00000478-199307000-00010. PMID 8317612.
- 1 2 3 4 5 Iwasaki T, Kawahara K, Nagano T, Nakagawa K (March 2007). "Pulmonary mucinous cystadenocarcinoma: an extremely rare tumor presenting as a cystic lesion of the lung". General Thoracic and Cardiovascular Surgery. 55 (3): 143–146. doi:10.1007/s11748-006-0089-z. PMID 17447515. S2CID 33648202.
- 1 2 3 Sezer O, Hoffmeier A, Bettendorf O, Franzius C, Semik M, Schmid C, Scheld HH (April 2006). "Mucinous cystadenocarcinoma--an extremely rare tumor in a young patient". The Thoracic and Cardiovascular Surgeon. 54 (3): 216–217. doi:10.1055/s-2005-872950. PMID 16639689. S2CID 260344527.
- ↑ Travis, W.D.; Colby, T.V.; Corrin, B. (1999). Histological Typing of Lung and Pleural Tumors. International histological classification of tumours, no. 1 (3rd ed.). Berlin: Springer. ISBN 978-3-540-65219-9.
- 1 2 3 Raza SA, Alexakis C, Creagh M, Lawrence DR, Wood M (August 2009). "Primary pulmonary mucinous cystadenocarcinoma presenting as a complex bronchocele: a case report". Journal of Medical Case Reports. 3: 8581. doi:10.4076/1752-1947-3-8581. PMC 2737758 . PMID 19830231.
- ↑ Butnor KJ, Sporn TA, Dodd LG (2001). "Fine needle aspiration cytology of mucinous cystadenocarcinoma of the lung: report of a case with radiographic and histologic correlation". Acta Cytologica. 45 (5): 779–783. doi:10.1159/000328305. PMID 11575661. S2CID 3339868.
- 1 2 Ishibashi H, Moriya T, Matsuda Y, Sado T, Hoshikawa Y, Chida M, et al. (November 2003). "Pulmonary mucinous cystadenocarcinoma: report of a case and review of the literature". The Annals of Thoracic Surgery. 76 (5): 1738–1740. doi: 10.1016/S0003-4975(03)00657-X . PMID 14602331.
- ↑ Gangopadhyay A, Bhattacharya M, Chatterjee SK, Barlow JJ, Tsukada Y (April 1985). "Immunoperoxidase localization of a high-molecular-weight mucin recognized by monoclonal antibody 1D3". Cancer Research. 45 (4): 1744–1752. PMID 3884144.
- 1 2 Gaeta M, Blandino A, Scribano E, Ascenti G, Minutoli F, Pandolfo I (1999). "Mucinous cystadenocarcinoma of the lung: CT-pathologic correlation in three cases". Journal of Computer Assisted Tomography. 23 (4): 641–643. doi:10.1097/00004728-199907000-00028. PMID 10433300.