Related Research Articles
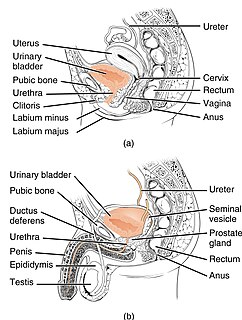
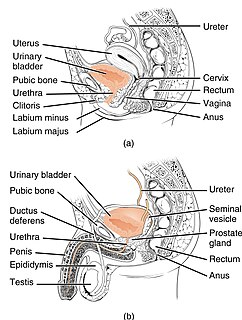
The urethra is a tube that connects the urinary bladder to the urinary meatus for the removal of urine from the body of both females and males. In human females and other primates, the urethra connects to the urinary meatus above the vagina, whereas in marsupials, the female's urethra empties into the urogenital sinus.
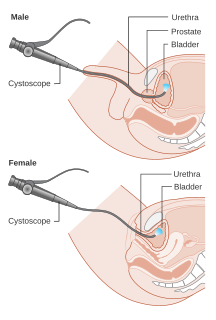
Cystoscopy is endoscopy of the urinary bladder via the urethra. It is carried out with a cystoscope.
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis.

Retrograde ejaculation occurs when semen which would be ejaculated via the urethra is redirected to the urinary bladder. Normally, the sphincter of the bladder contracts before ejaculation, sealing the bladder which besides inhibiting the release of urine also prevents a reflux of seminal fluids into the male bladder during ejaculation. The semen is forced to exit via the urethra, the path of least resistance. When the bladder sphincter does not function properly, retrograde ejaculation may occur. It can also be induced deliberately by a male as a primitive form of male birth control or as part of certain alternative medicine practices. The retrograde-ejaculated semen, which goes into the bladder, is excreted with the next urination.

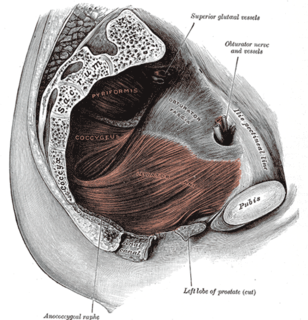
The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region below. Both males and females have a pelvic floor. To accommodate the birth canal, a female's pelvic cavity is larger than a male's.

Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladder control, mild lower abdominal pain, and a weak urine stream. Those with long-term problems are at risk of urinary tract infections.

A cystocele, also known as a prolapsed bladder, is a medical condition in which a woman's bladder bulges into her vagina. Some may have no symptoms. Others may have trouble starting urination, urinary incontinence, or frequent urination. Complications may include recurrent urinary tract infections and urinary retention. Cystocele and a prolapsed urethra often occur together and is called a cystourethrocele. Cystocele can negatively affect quality of life.

Radical retropubic prostatectomy is a surgical procedure in which the prostate gland is removed through an incision in the abdomen. It is most often used to treat individuals who have early prostate cancer. Radical retropubic prostatectomy can be performed under general, spinal, or epidural anesthesia and requires blood transfusion less than one-fifth of the time. Radical retropubic prostatectomy is associated with complications such as urinary incontinence and impotence, but these outcomes are related to a combination of individual patient anatomy, surgical technique, and the experience and skill of the surgeon.
Stress incontinence, also known as stress urinary incontinence (SUI) or effort incontinence is a form of urinary incontinence. It is due to inadequate closure of the bladder outlet by the urethral sphincter.
Neurogenic bladder dysfunction, or neurogenic bladder, refers to urinary bladder problems due to disease or injury of the central nervous system or peripheral nerves involved in the control of urination. There are multiple types of neurogenic bladder depending on the underlying cause and the symptoms. Symptoms include overactive bladder, urinary urgency, frequency, incontinence or difficulty passing urine. A range of diseases or conditions can cause neurogenic bladder including spinal cord injury, multiple sclerosis, stroke, brain injury, spina bifida, peripheral nerve damage, Parkinson's disease, or other neurodegenerative diseases. Neurogenic bladder can be diagnosed through a history and physical as well as imaging and more specialized testing. Treatment depends on underlying disease as well as symptoms and can be managed with behavioral changes, medications, surgeries, or other procedures. The symptoms of neurogenic bladder, especially incontinence, can have a significant impact on quality of life.
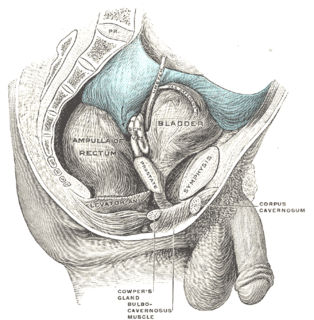
Retropubic space is a potential avascular space located between the pubic symphysis and the urinary bladder. The retropubic space is a preperitoneal space, located behind the transversalis fascia and in front of peritoneum.

The urethral sphincters are two muscles used to control the exit of urine in the urinary bladder through the urethra. The two muscles are either the male or female external urethral sphincter and the internal urethral sphincter. When either of these muscles contracts, the urethra is sealed shut.
A urethrocele is the prolapse of the female urethra into the vagina. Weakening of the tissues that hold the urethra in place may cause it to protrude into the vagina. Urethroceles often occur with cystoceles. In this case, the term used is cystourethrocele.
Urogynecology or urogynaecology is a surgical sub-specialty of urology and gynecology.

Urodynamic testing or urodynamics is a study that assesses how the bladder and urethra are performing their job of storing and releasing urine. Urodynamic tests can help explain symptoms such as:

Overflow incontinence is a form of urinary incontinence, characterized by the involuntary release of urine from an overfull urinary bladder, often in the absence of any urge to urinate. This condition occurs in people who have a blockage of the bladder outlet, or when the muscle that expels urine from the bladder is too weak to empty the bladder normally. Overflow incontinence may also be a side effect of certain medications.

An artificial urinary sphincter (AUS) is an implanted device to treat moderate to severe stress urinary incontinence, most commonly in men. The AUS is designed to supplement the function of the natural urinary sphincter that restricts urine flow out of the bladder.
A urethral diverticulum is a condition where the urethra or the periurethral glands push into the connective tissue layers (fascia) that surround it.
Urethral hypermobility is a condition of excessive movement of the female urethra due to a weakened urogenital diaphragm. It describes the instability of the urethra in relation to the pelvic floor muscles. A weakened pelvic floor muscle fails to adequately close the urethra and hence can cause stress urinary incontinence. This condition can be measured with anterior compartment descent. It is sometimes treated with urethral bulking injections.

If medical treatment is not effective, surgery may need to be performed for benign prostatic hyperplasia.
References
- Hoffman, Barbara (2012). Williams gynecology, 2nd edition. New York: McGraw-Hill Medical. pp. 1198–1199. ISBN 0071716726. 1 2 3 4 5 Walters, Mark (2015). Urogynecology and reconstructive pelvic surgery, Chapter 22. Philadelphia, PA: Elsevier/Saunders. ISBN 9780323113779; Access provided by the University of Pittsburgh
- ↑ Hoffman, Barbara (2012). Williams gynecology, 2nd edition. New York: McGraw-Hill Medical. pp. 1198–1199. ISBN 978-0071716727.
- 1 2 3 4 5 Walters, Mark (2015). Urogynecology and reconstructive pelvic surgery, Chapter 22. Philadelphia, PA: Elsevier/Saunders. ISBN 9780323113779; Access provided by the University of Pittsburgh
{{cite book}}: CS1 maint: postscript (link)